110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

冠状动脉疾病老年患者高阿司匹林 (Aspirin) 血小板反应性的预测因子
Authors Zhang JW, Liu WW, McCaffrey TA, He XQ, Liang WY, Chen XH, Feng XR, Fu SW, Liu ML
Received 1 April 2017
Accepted for publication 18 June 2017
Published 10 August 2017 Volume 2017:12 Pages 1271—1279
DOI https://doi.org/10.2147/CIA.S138592
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Akshita Wason
Peer reviewer comments 3
Editor who approved publication: Professor Zhi-Ying Wu
Objectives: Previous studies have illustrated the link between high on-aspirin
platelet reactivity (HAPR) with increasing thrombotic risks. The aim of our
study was to investigate relative risk factors of HAPR in elderly patients with
coronary artery disease.
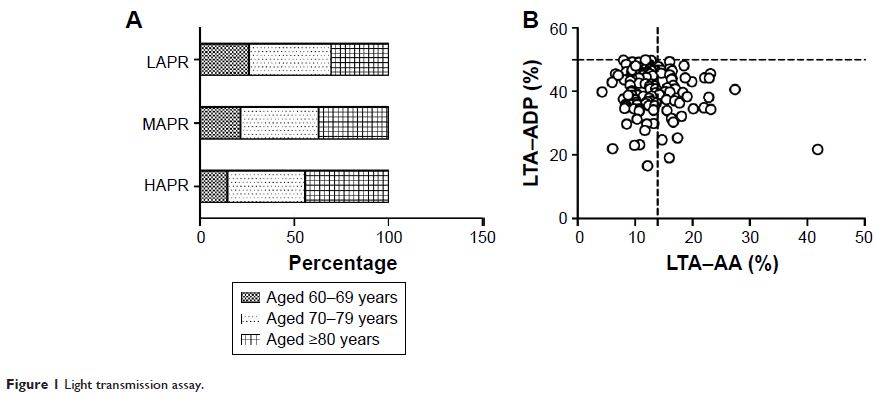
Methods: Elderly, hospitalized coronary artery disease patients
on regular aspirin treatment were enrolled from January 2014 to September 2016.
Medical records of each patient were collected, including demographic
information, cardiovascular risk factors, concomitant drugs and routine
biological parameters. Arachidonic acid (AA, 0.5 mg/mL) and adenosine
diphosphate (ADP, 5 µmol/L) induced platelet aggregation were measured via
light transmission assay (LTA) to evaluate antiplatelet responses, referred as
LTA–AA and LTA–ADP.
Results: A total of 275 elderly patients were included,
with mean age of 77.2±8.1 years, and males accounted for 81.8%. HAPR was
defined as LTA–AA in the upper quartile of the enrolled population. HAPR
patients tended to have lower renal function (P =0.052).
Higher serum uric acid (SUA) level, as well as lower platelet count, hemoglobin
and hematocrit were observed in HAPR patients, with a higher proportion of
diuretics use (P <0.05). Multivariate analysis
revealed that SUA (OR: 1.004, 95% CI: 1.000–1.007, P =0.048), platelet count (OR:
0.994, 95% CI: 0.989–1.000, P =0.045),
hematocrit (OR: 0.921, 95% CI: 0.864–0.981, P =0.011)
and concomitant P2Y12 receptor inhibitors use (OR: 1.965, 95% CI:
1.075–3.592, P =0.028) were correlated with
HAPR. Spearman’s correlation analysis demonstrated an inverse association of
LTA–AA with hematocrit (r =−0.234, P <0.001), hemoglobin (r =−0.209, P <0.001) and estimated
glomerular filtration rate (r =−0.132, P =0.031).
Conclusion: SUA, platelet count, hematocrit and P2Y12 receptor
inhibitors use were independently correlated with HAPR. These parameters might
provide novel therapeutic targets for optimizing antiplatelet therapy.
Keywords: aspirin,
platelet reactivity, elderly, risk factors, coronary artery disease