110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

Capillary PO2 does not adequately reflect arterial PO2 in hypoxemic COPD patients
Authors Magnet FS, Majorski DS, Callegari J, Schwarz SB, Schmoor C, Windisch W, Storre JH
Received 1 May 2017
Accepted for publication 19 June 2017
Published 6 September 2017 Volume 2017:12 Pages 2647—2653
DOI https://doi.org/10.2147/COPD.S140843
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Charles Downs
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Purpose: To
compare arterial (PaO2) with capillary (PcO2) partial pressure of
oxygen in hypoxemic COPD patients because capillary blood gas analysis (CBG) is
increasingly being used as an alternative to arterial blood gas analysis (ABG)
in a non-intensive care unit setting, although the agreement between PcO2 and PaO2 has not been
evaluated in hypoxemic COPD patients.
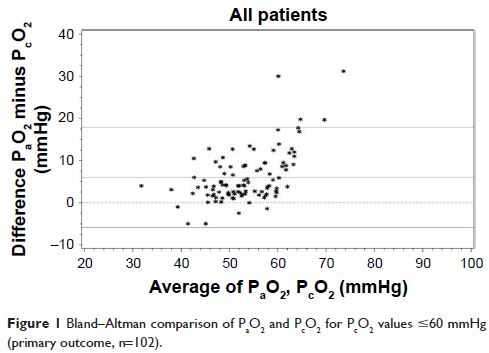
Patients and
methods: Bland–Altman comparison of PaO2 and PcO2 served as the
primary outcome parameter if PcO2 values were ≤60
mmHg and the secondary outcome parameter if PcO2 values were ≤55
mmHg. Pain associated with the measurements was assessed using a 100-mm visual
analog scale.
Results: One hundred and two PaO2/PcO2 measurement pairs
were obtained. For PcO2 values ≤60 mmHg,
the mean difference between PaO2 and PcO2 was 5.99±6.05
mmHg (limits of agreement: -5.88 to 17.85 mmHg). For PcO2 values ≤55 mmHg
(n=73), the mean difference was 5.33±5.52 mmHg (limits of agreement: -5.48 to
16.15 mmHg). If PaO2 ≤55 (≤60) mmHg
was set as the cut-off value, in 20.6% (30.4%) of all patients, long-term
oxygen therapy have been unnecessarily prescribed if only PcO2 would have been
assessed. ABG was rated as more painful compared with CBG.
Conclusions: PcO2 does not adequately reflect PaO2 in hypoxemic COPD
patients, which can lead to a relevant number of unnecessary long-term oxygen
therapy prescriptions.
Keywords: blood gas analysis, COPD, respiratory insufficiency, hypoxemia