108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

Comorbidity index in central cancer registries: the value of hospital discharge data
Authors Lichtensztajn DY, Giddings BM, Morris CR, Parikh-Patel A, Kizer KW
Received 14 July 2017
Accepted for publication 26 September 2017
Published 20 November 2017 Volume 2017:9 Pages 601—609
DOI https://doi.org/10.2147/CLEP.S146395
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Lucy Goodman
Peer reviewer comments 2
Editor who approved publication: Professor Henrik Toft Sørensen
Background: The presence of comorbid medical conditions can significantly affect a
cancer patient’s treatment options, quality of life, and survival. However,
these important data are often lacking from population-based cancer registries.
Leveraging routine linkage to hospital discharge data, a comorbidity score was
calculated for patients in the California Cancer Registry (CCR) database.
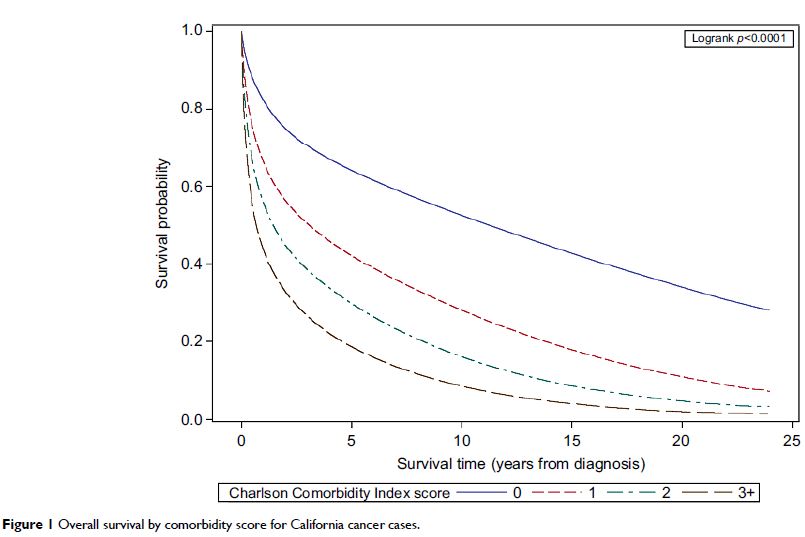
Methods: California cancer cases diagnosed between 1991 and 2013 were
linked to statewide hospital discharge data. A Deyo and Romano adapted Charlson
Comorbidity Index was calculated for each case, and the association of
comorbidity score with overall survival was assessed with Kaplan–Meier curves
and Cox proportional hazards models. Using a subset of Medicare-enrolled CCR
cases, the index was validated against a comorbidity score derived using
Surveillance, Epidemiology, and End Results (SEER)-Medicare linked data.
Results: A comorbidity score was calculated for 71% of CCR cases. The majority
(60.2%) had no relevant comorbidities. Increasing comorbidity score was
associated with poorer overall survival. In a multivariable model, high
comorbidity conferred twice the risk of death compared to no comorbidity
(hazard ratio 2.33, 95% CI: 2.32–2.34). In the subset of patients with a
SEER-Medicare-derived score, the sensitivity of the hospital discharge-based
index for detecting any comorbidity was 76.5. The association between overall
mortality and comorbidity score was stronger for the hospital discharge-based
score than for the SEER-Medicare-derived index, and the predictive ability of
the hospital discharge-based score, as measured by Harrell’s C index, was also
slightly better for the hospital discharge-based score (C index 0.62 versus
0.59, P <0.001).
Conclusions: Despite some limitations, using hospital discharge data to
construct a comorbidity index for cancer registries is a feasible and valid
method to enhance registry data, which can provide important clinically
relevant information for population-based cancer outcomes research.
Keywords: administrative health care data, data linkages, population-based,
validation, cancer registry, hospital discharge data, survival