111446
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

在进行视频辅助的胸腔镜肺癌肺叶切除术后,肺裂隙完整度对院内治疗效果的影响:一个回顾性队列研究
Authors Li S, Wang Z, Zhou K, Wang Y, Wu Y, Li P, Che G
Received 12 December 2017
Accepted for publication 27 January 2018
Published 2 March 2018 Volume 2018:14 Pages 461—474
DOI https://doi.org/10.2147/TCRM.S159632
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 2
Editor who approved publication: Professor Deyun Wang
Background: To evaluate the clinical significance of degree of pulmonary
fissure completeness (PFC) on major in-hospital outcomes following
video-assisted thoracoscopic (VATS) lobectomy for non-small-cell lung cancer
(NSCLC).
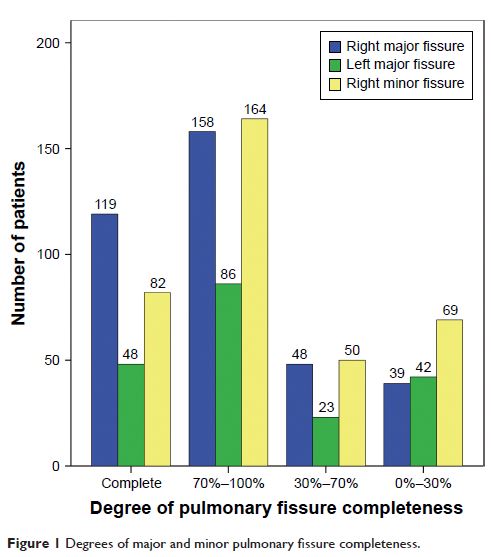
Materials and methods: We carried out a single-center retrospective analysis
on the prospectively maintained database at our unit between August 2014 and
October 2015. Patients were divided into two groups based on their fissure sum
average (FSA). Patients with FSA >1 (1< FSA ≤3) were considered to have
incomplete pulmonary fissures (group A), while patients with FSA of 0–1 were
considered to have complete pulmonary fissures (group B). Demographic
differences in perioperative characteristics and surgical outcomes between
these two groups were initially assessed. Then, a multivariate
logistic-regression analysis was further conducted to identify the independent
predictors for major in-hospital outcomes.
Results: A total of 563 patients undergoing VATS lobectomy for
NSCLC were enrolled. There were 190 patients in group A and 373 patients in
group B. The overall morbidity and mortality rates of our cohort were 30.6% and
0.5%, respectively. Group A patients had a significantly higher overall morbidity
rate than group B patients (42.1% vs 24.7%, P <0.001).
Both minor morbidity (40.5% vs 22%, P <0.001) and
major morbidity (11.1% vs 5.6%, P =0.021) rates in
group A patients were also significantly higher than group B patients. No
significant difference was observed in mortality rate between these two groups
(1.1% vs 0.3%, P =0.26). The
incomplete degree of PFC was significantly correlated with length of stay and
chest-tube duration (log-rank P <0.001) after
surgery. Finally, the incomplete degree of PFC was found to be predictive of
overall morbidity (OR 2.08, P <0.001), minor
morbidity (OR 2.39, P <0.001), and
major morbidity (OR 2.06, P =0.031) by
multivariate logistic-regression analyses.
Conclusion: Degree of PFC is an excellent categorical
predictor for both major and minor morbidity after VATS lobectomy for NSCLC.
Keywords: pulmonary
fissure completeness, video-assisted thoracoscopic surgery, lobectomy,
non-small-cell lung cancer, morbidity, mortality