108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

根治性前列腺切除术和外照射放疗治疗临床局部高危前列腺癌的生存结果: 基于人群的倾向评分匹配研究
Authors Gu X, Gao X, Cui M, Xie M, Ma M, Qin S, Li X, Qi X, Bai Y, Wang D
Received 18 November 2017
Accepted for publication 19 March 2018
Published 8 May 2018 Volume 2018:10 Pages 1061—1067
DOI https://doi.org/10.2147/CMAR.S157442
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Justinn Cochran
Peer reviewer comments 2
Editor who approved publication: Professor Kenan Onel
Objective: This study was aimed to compare survival outcomes in high-risk
prostate cancer (PCa) patients receiving external beam radiotherapy (EBRT) or
radical prostatectomy (RP).
Materials and
methods: The Surveillance, Epidemiology, and
End Results (SEER) database was used to identify PCa patients with high-risk
features who received RP alone or EBRT alone from 2004 to 2008.
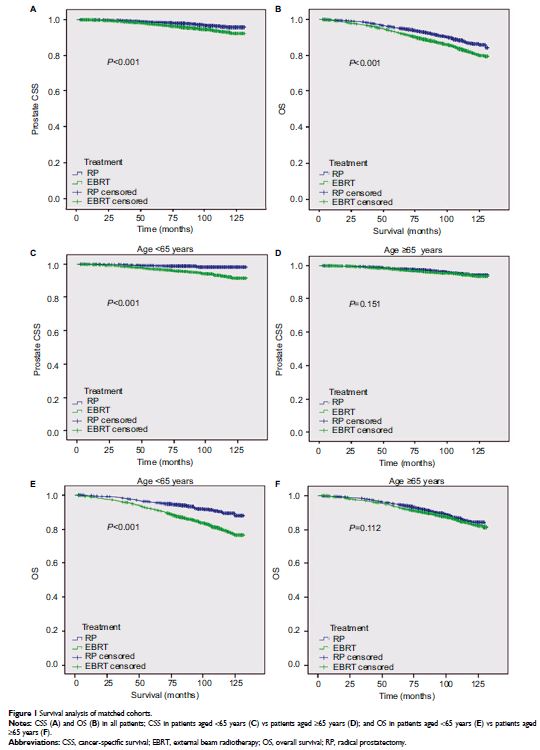
Propensity-score matching (PSM) was performed. Kaplan–Meier survival analysis
was used to compare cancer-specific survival (CSS) and overall survival (OS).
Multivariate Cox regression analysis was used to identify independent
prognostic factors.
Results: A total of 24,293 patients were identified, 14,460 patients receiving RP
and 9833 patients receiving EBRT. Through PSM, 3828 patients were identified in
each group. The mean CSS was 128.6 and 126.7 months for RP and EBRT
groups, respectively (P <0.001). The
subgroup analyses showed that CSS of the RP group was better than that of the
EBRT group for patients aged <65 years (P <0.001),
White race (P <0.001), and married status (P <0.001). However, there was no
significant difference in CSS for patients aged ≥65 years, Black race,
other race, and unmarried status. Similar trends were observed for OS.
Multivariate analysis showed that EBRT treatment modality, T3–T4 stage, Gleason
score 8–10, and prostate-specific antigen >20 ng/mL were significant
risk factors for both CSS and OS.
Conclusion: This study suggested that survival outcomes might be better with
RP than EBRT in high-risk PCa patients aged <65 years; however, RP and
EBRT provided equivalent survival outcomes in older patients, which argues for
primary radiotherapy in this older cohort.
Keywords: prostate cancer, SEER, radical prostatectomy, EBRT