108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

术前血清载脂蛋白 A-I 水平可预测非肌层浸润性膀胱癌患者的长期生存率
Authors Shang Z, Wang J, Wang X, Yan H, Cui B, Jia C, Wang Q, Cui X, Li J, Ou T
Received 10 February 2018
Accepted for publication 17 March 2018
Published 14 May 2018 Volume 2018:10 Pages 1177—1190
DOI https://doi.org/10.2147/CMAR.S165213
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 2
Editor who approved publication: Professor Nakshatri
Introduction: The aim of this study was to elucidate the association between
apolipoprotein A-I (Apo A-I) and overall survival (OS) as well as
cancer-specific survival (CSS) in non-muscle-invasive bladder cancer (NMIBC)
patients undergoing transurethral resection of bladder tumor (TURBT).
Patients and
methods: We retrospectively collected data of
470 eligible patients diagnosed with NMIBC and who received TURBT between
January 2004 and December 2011. Pretreatment blood indexes were examined. The
association of Apo A-I with clinicopathological characteristics was further
analyzed by dichotomizing our sample into those with Apo A-I ≤ 1.19 g/L (low
Apo A-I group) and those with Apo A-I > 1.19 g/L (high Apo A-I group). OS
and CSS were estimated by Kaplan–Meier analysis and the log-rank test was used
to compare differences between groups. Univariate and multivariate Cox
regression analyses were plotted to assess the prognostic value of Apo A-I in
NMIBC patients. In addition, subgroup analyses were performed according to the
risk classification of the International Bladder Cancer Group.
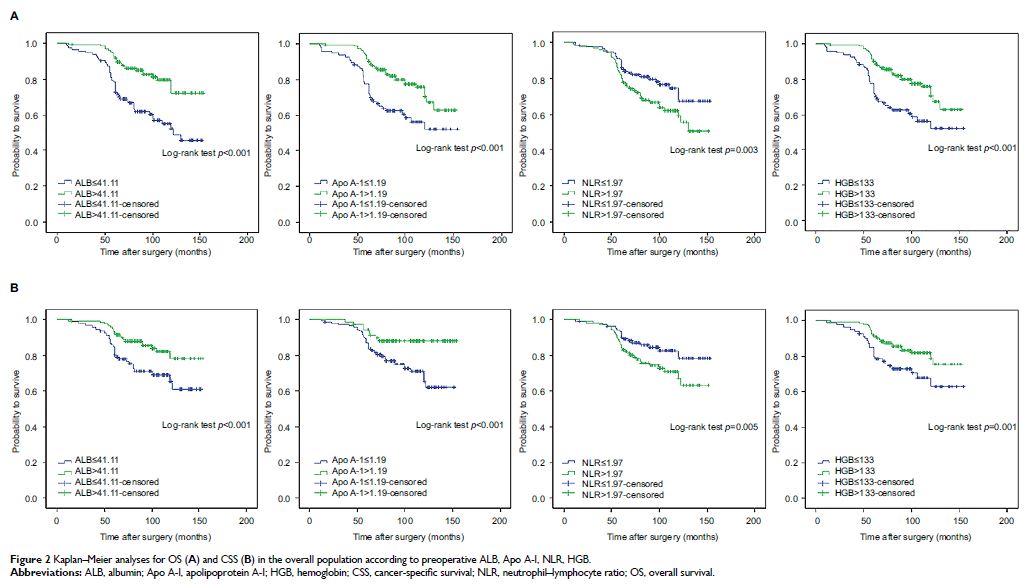
Results: In the overall population, patients in the high Apo A-I group had
greater 5-year OS and 5-year CSS rates as compared to those in the low Apo A-I
group. Kaplan–Meier survival analysis revealed that higher albumin, Apo A-I,
and hemoglobin levels were associated with greater OS and CSS while elevated
neutrophil–lymphocyte ratio was associated with worse OS and CSS in the overall
and high-risk population rather than low- and intermediate-risk population.
Furthermore, Apo A-I was shown to be an independent predictor in the overall
population (for OS, hazard ratio [HR], 0.364, 95% confidence interval [CI],
0.221–0.598, p < 0.001; for CSS, HR,
0.328, 95% CI, 0.185–0.583, p < 0.001) and
high-risk patients (for OS, HR, 0.232, 95% CI 0.121–0.443, p < 0.001; for CSS, HR,
0.269, 95% CI, 0.133–0.541, p < 0.001).
Conclusion: These results suggest that Apo A-I level could potentially serve
as a useful prognostic indicator for therapeutic decision making in NMIBC
patients.
Keywords: apolipoprotein A-I, NMIBC, TURBT, prognosis, overall survival,
cancer-specific survival