108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

平足蛋白的表达增多及其在鳞状非小细胞肺癌中的临床病理、预后和治疗价值
Authors Xie L, Lin C, Zhang Q, Piao H, Bigner DD, Zhang Z, Bao X
Received 23 January 2018
Accepted for publication 20 March 2018
Published 24 May 2018 Volume 2018:10 Pages 1329—1340
DOI https://doi.org/10.2147/CMAR.S163510
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 2
Editor who approved publication: Professor Nakshatri
Background: Squamous non-small cell lung cancer (SqNSCLC), as a leading cause
of cancer-related deaths worldwide, has limited treatment options and poor
prognosis. Thus, novel targeted therapies are desperately needed.
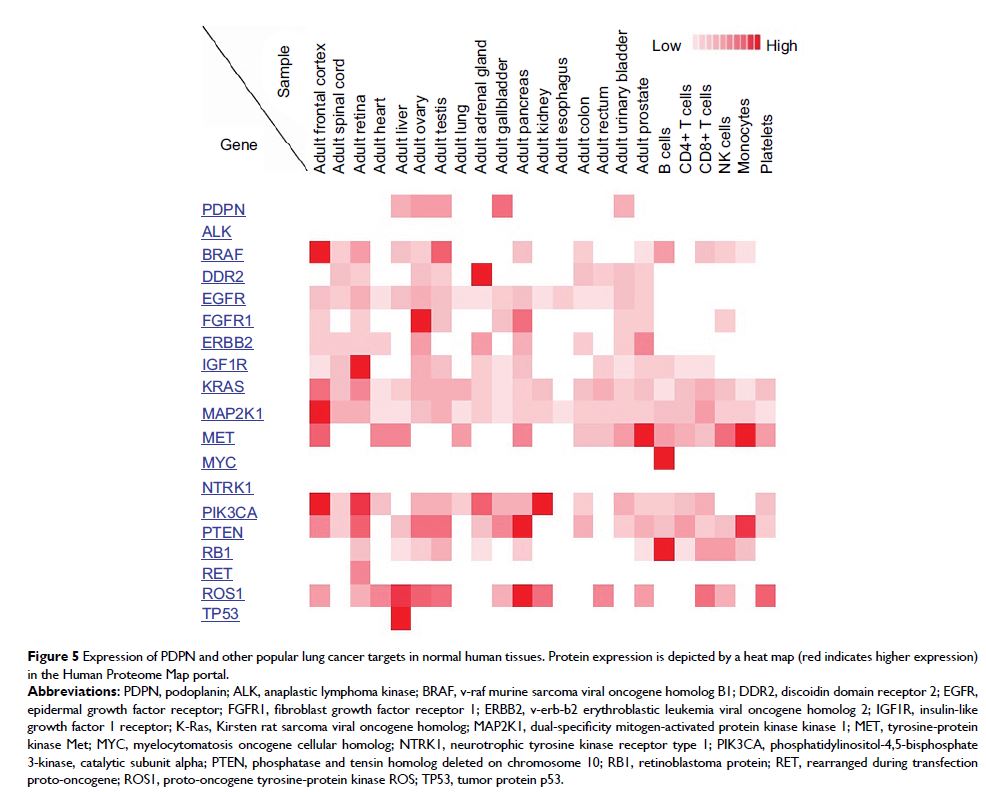
Materials and methods: SqNSCLC cases from derivation and validation
cohorts were analyzed for podoplanin (PDPN) expression, and its
clinicopathological correlation and prognostic prediction. The Human Proteome
Map database was used to compare the expression of different lung cancer
targets in normal human tissues. Two human lung cancer cell lines, H226 (a
SqNSCLC line) and A549 (a non-SqNSCLC line), were examined for PDPN expression.
The in vitro cytotoxicity of an anti-PDPN therapy (NZ-1-immunotoxin [NZ-1-IT])
was tested against both lines. The in vivo therapeutic effect of NZ-1-IT was
examined in subcutaneous non-small cell lung cancer (NSCLC) xenograft mouse
models.
Results: In the derivation cohort, 40% (28/70) were PDPN
positive. There was significantly increasing pleural invasion (46.4% vs
9.5%, p =0.001), lymphovascular invasion
(25.0% vs 9.5%, p =0.08), and lymph
node involvement (53.6% vs 33.3%, p =0.09) in
PDPN-positive vs PDPN-negative patients, along with poorer progression-free
survival in PDPN-positive patients (p =0.07). The
validation cohort with 224 randomly matched cases from The Cancer Genome Atlas
data set also displayed significantly shorter overall survival in the group
with elevated PDPN mRNA (p =0.05). However, PDPN showed
limited expression in normal tissues. PDPN was highly and specifically
expressed on the surface of H226 cells instead of A549 cells. Subsequently,
PDPN-positive H226 cells were around 800 times more sensitive to anti-PDPN
NZ-1-IT therapy than PDPN-negative A549 cells in vitro. Furthermore, NZ-1-IT
significantly delayed tumorigenesis only in the H226 subcutaneous mouse model (p <0.05).
Conclusion: Our results demonstrate a distinctively elevated
expression of PDPN in SqNSCLC, which is significantly associated with worse
clinicopathological features and poorer prognosis. With promising preclinical
therapeutic results, anti-PDPN targeted therapy can thus be a robust potential
strategy for future SqNSCLC treatment.
Keywords: podoplanin,
squamous non-small cell lung cancer, pleural invasion, prognosis, molecular
targeted therapy, immunotoxins