108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

抗菌治疗的最佳输注率:过去五年来证据大爆炸
Authors Zhu LL, Zhou Q
Received 8 March 2018
Accepted for publication 13 June 2018
Published 8 August 2018 Volume 2018:11 Pages 1105—1117
DOI https://doi.org/10.2147/IDR.S167616
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 3
Editor who approved publication: Dr Eric Nulens
Background: Sporadic studies in antimicrobial therapy have evaluated the
effects of infusion rates on therapeutic and economic outcomes, and new findings
may challenge the regular infusion regimen.
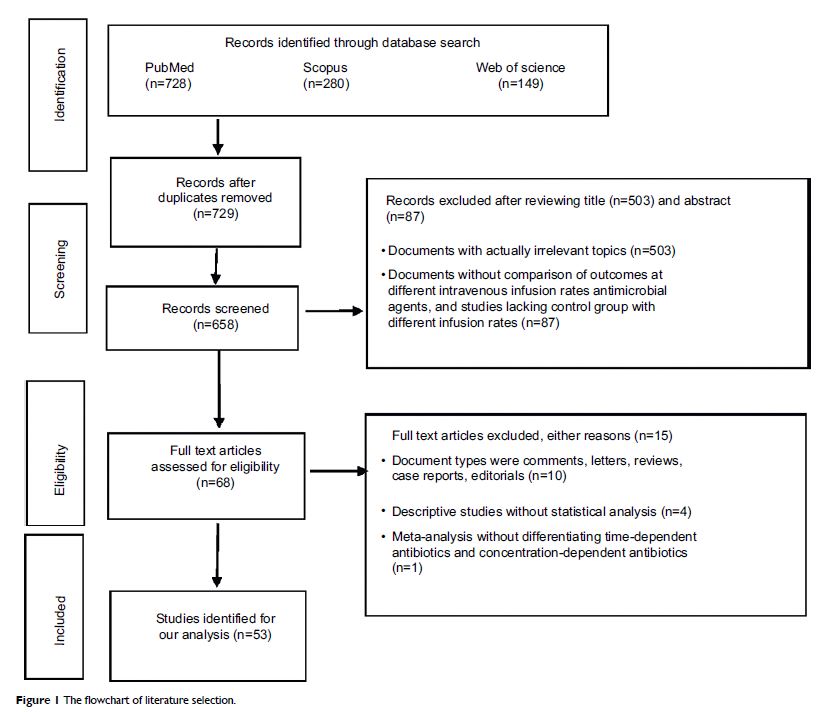
Methods: Focusing on studies comparing the outcomes of different infusion
regimens, the relevant literature was identified by searching PubMed, Web of
Science, and Scopus from January 1, 2013 to March 1, 2018. Papers were finally
chosen using a PRISMA flowchart.
Results: Antimicrobials with the superiority of prolonged infusion to
standard infusion in terms of efficacy and safety include meropenem, doripenem,
imipenem, cefepime, ceftazidime, piperacillin/tazobactam, linezolid, and
vancomycin. The strategy of concomitantly reducing total daily dose and
prolonging infusion time may cause treatment failure (eg, imipenem). Extended
infusion of piperacillin/tazobactam has pharmacoeconomic advantage over standard
infusion. Prolonged infusion of voriconazole is inferior to standard infusion
because of lower efficacy caused by pharmacokinetic changes. Comparable
outcomes following standard infusion and continuous infusion were observed with
norvancomycin and nafcillin. Factors determining whether prolonged infusion has
a benefit over standard infusion include MIC of bacterial pathogens, bacterial
density, diagnosis, disease severity, total daily dose, and renal function.
Conclusion: To maximally preserve the effectiveness of current antimicrobials,
effective interventions should be implemented to enhance the application of
optimal infusion strategies. For reducing nephrotoxicity, prolonged infusion of
meropenem is better than conventional infusion in neonates with Gram-negative
late-onset sepsis, and continuous infusion of vancomycin is superior to
intermittent infusion. For increasing efficacy, prolonged or continuous
infusion of time-dependent antimicrobials (eg, meropenem, doripenem, imipenem,
cefepime, ceftazidime, piperacillin/tazobactam, linezolid, and vancomycin) is
an optimal choice. Nevertheless, such advantages may only be demonstrated in
special clinical circumstances and special populations (eg, patients with a
sequential organ failure assessment (SOFA) score≥9, respiratory tract
infections, urinary or intra-abdominal infections, or infections caused by less
susceptible pathogens would benefit from prolonged infusion of
piperacillin/tazobactam).
Keywords: antimicrobial resistance, antimicrobial stewardship, efficacy,
infection, infusion regimen, nursing time, safety, pharmacoeconomics