111446
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

可切除的胰腺导管腺癌术前炎症标志物预后评分价值的比较和验证
Authors Ye S, Bai L
Received 8 May 2018
Accepted for publication 11 July 2018
Published 11 September 2018 Volume 2018:10 Pages 3405—3417
DOI https://doi.org/10.2147/CMAR.S173444
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
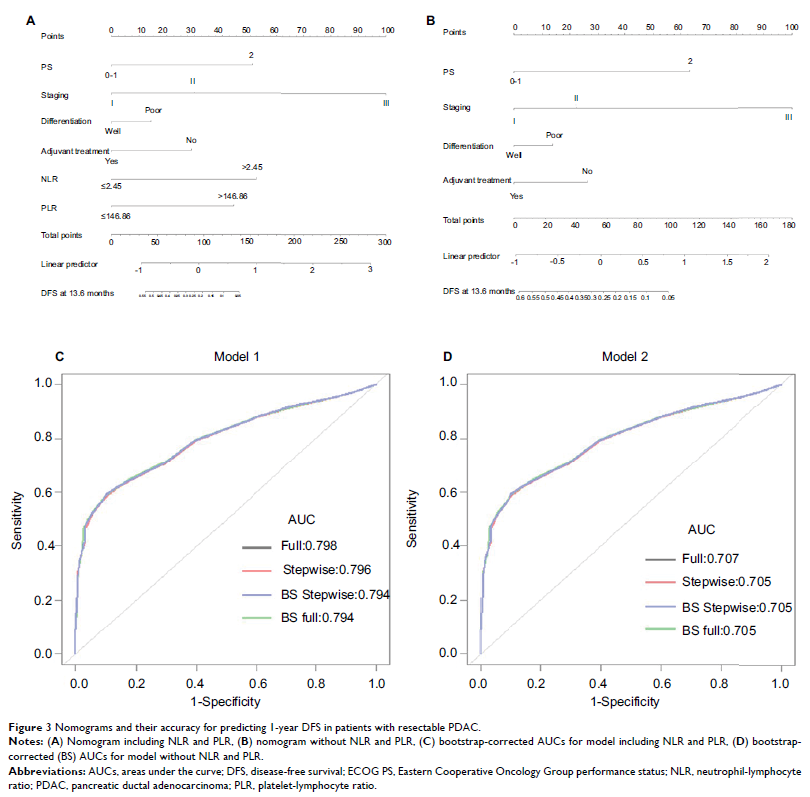
Purpose: We aimed to compare and validate the prognostic value of inflammation-based prognostic scores for patients with resectable pancreatic ductal adenocarcinoma (PDAC) and to establish a novel, effective nomogram incorporating inflammation-based prognostic scores to predict disease-free survival (DFS) in these patients.
Patients and methods: Clinicopathological characteristics and follow-up data were retrieved from our prospective database. A total of 420 patients with PDAC who underwent radical resection were evaluated between January 2007 and December 2016. Blood samples were obtained within 7 days prior to surgical intervention. Time-dependent receiver operating characteristic curves were generated to determine optimal cutoff values for independent prognostic factors. Nomograms for DFS were established based on multivariate Cox proportional hazard models, and the results were internally validated using bootstrap resampling.
Results: Neutrophil-lymphocyte ratio (NLR) >2.13 and platelet-lymphocyte ratio (PLR) >140 were independent prognostic factors for DFS and overall survival. Stratified analyses indicated that these associations were not present among patients with stage III disease. Independent predictors of DFS, including Eastern Cooperative Oncology Group performance status score, tumor stage, differentiation, adjuvant treatment, NLR, and PLR, were incorporated into two nomograms for prediction of DFS in a cohort of PDAC patients after curative surgery. The area under receiver operating characteristic curve of the nomogram including NLR and PLR (0.804) was higher than that without NLR and PLR (0.711). The bootstrap-corrected AUC for the model including NLR and PLR was 0.803, while that for the model without NLR and PLR was 0.711.
Conclusion: Our study demonstrates that high NLR and high PLR are important clinical predictors of poor survival in patients with resectable PDAC. Additionally, a nomogram including NLR and PLR can objectively and reliably predict DFS among patients with PDAC following curative surgery.
Keywords: neutrophil-lymphocyte ratio, NLR, platelet-lymphocyte ratio, PLR, nomogram, disease-free survival