108605
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

术前血清炎症标志物升高会增加骨关节炎患者全膝关节置换术后假体周围关节感染的风险
Authors Xu C, Guo H, Qu PF, Fu J, Kuo FC, Chen JY
Received 31 May 2018
Accepted for publication 23 July 2018
Published 17 September 2018 Volume 2018:14 Pages 1719—1724
DOI https://doi.org/10.2147/TCRM.S175854
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Justinn Cochran
Peer reviewer comments 2
Editor who approved publication: Professor Deyun Wang
Background: The purpose of this study was to evaluate the prevalence of
preoperatively elevated serum inflammatory markers and to determine its
association with periprosthetic joint infection (PJI) in patients with osteoarthritis
(OA) undergoing total knee arthroplasty (TKA).
Methods: From January 2010 to May 2014, we retrospectively reviewed 3,376
consecutive patients who were scheduled for unilateral TKA due to OA. Patients
with inflammatory arthritis, posttraumatic arthritis, previous knee surgery,
simultaneous surgery or arthroplasty, and comorbidity with autoimmune disease,
hepatitis, renal disease, respiratory tract infections, urinary tract
infection, and malignancy were excluded. One hundred and forty patients with
preoperatively elevated erythrocyte sedimentation rate (ESR) or C-reactive
protein (CRP) were enrolled. The control group was matched by age, sex, body
mass index, and year of index surgery in 1:1 ratio. All patients were followed
for a minimum of 1 year or until the occurrence of PJI. PJI was defined based
on the criteria in the International Consensus Meeting. A multivariate Cox
proportional hazards model was utilized to calculate the HR and 95% CI.
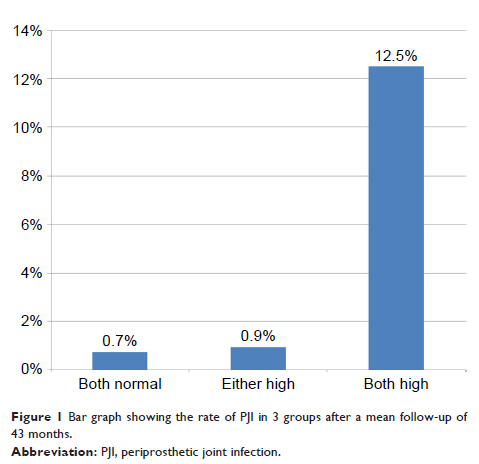
Results: The prevalence of preoperatively elevated inflammatory markers was
4.1%. The rate of PJI was significantly higher in the both elevated ESR and CRP
groups (12.5%, 4/32) compared with both normal group (1.4%, 2/140) and either
high group (0.9%, 1/108) (P <0.001).
Patients with preoperative elevated ESR and CRP had a significant risk of PJI
compared to those with normal serum inflammatory markers (HR: 15.8, 95% CI:
2.57–96.7, P =0.003) after adjusting
confounding factors. The cumulative rate for PJI was 6.3% (95% CI: 0%–14.27%)
at 1 year and 16.5% (95% CI: 0%–30.66%) at 5 years for both high ESR and CRP
groups, which was significantly higher than other 2 groups (P =0.0002).
Conclusion: Although the prevalence of preoperatively elevated ESR and CRP is
low, routine examination of ESR and CRP preoperatively might be necessary to
prevent subsequent PJI in patients with OA following TKA.
Keywords: erythrocyte sedimentation rate, C-reactive protein, periprosthetic
joint infection, total knee arthroplasty, osteoarthritis