110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

在晚期胃食管癌中使用靶向药物是否会增加完全反应?对 18 项随机对照试验的综合分析
Authors Pang Y, Shen Z, Sun J, Wang W
Received 14 May 2018
Accepted for publication 24 July 2018
Published 12 November 2018 Volume 2018:10 Pages 5505—5514
DOI https://doi.org/10.2147/CMAR.S174063
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 3
Editor who approved publication: Dr Antonella D'Anneo
Purpose: We aimed to investigate whether the use
of targeted agents (TAs) in advanced gastroesophageal cancer (GEC) increased
the complete response (CR) and to assess the surrogate endpoints for survival
in the targeted treatment of GEC by using a meta-analysis of randomized
controlled trials (RCTs).
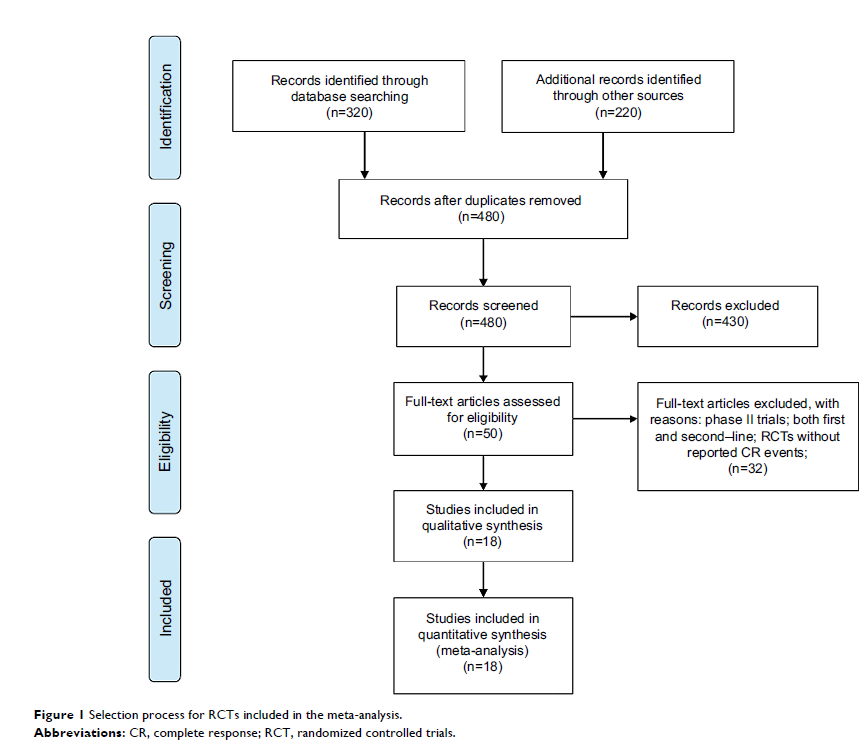
Methods: Eligible
studies were identified using Medline, PubMed, and meeting abstracts. Searches
were last updated on April 30, 2018. We calculated the incidence and Peto odds
ratio (Peto OR) of CR events in patients assigned to TAs compared with
controls. Simple linear regression models were fitted for median overall
survival (OS) and each surrogate [median progression-free survival (PFS), CRs,
objective response rate (ORR), and disease control rate (DCR), respectively].
Results: A
total of 7,892 GEC patients from 18 RCTs were included for analysis. The
incidence of CR in GEC patients treated with TAs was 2.0% (95% CI, 1.3%–3.0%)
compared with 1.7% (95% CI, 1.0%–2.7%) in the control arms. The use of TAs in
advanced GEC had a tendency to improve the possibility of archiving CR (Peto OR
1.42; 95% CI, 0.98–2.04; P =0.064) compared with controls. Subgroup analysis
according to treatment TAs showed that the addition of antiepidermal growth
factor receptor (EGFR) agents to chemotherapy in GEC significantly improved the
CR rate in comparison with control (Peto OR 1.77; 95% CI, 1.02–3.09; P =0.044), but not
for other molecular TAs (P =0.49 for angiogenesis inhibitors, P =0.66 for
mesenchymal-epithelial transition inhibitors). We also found that the addition
of TAs to first-line therapy (Peto OR 1.41; 95% CI, 0.94–2.11; P =0.098) had a
tendency to increase the chance of obtaining a CR, but not for second-line
therapy (Peto OR 1.47; 95% CI, 0.60–3.55; P =0.40). In
addition, correlation analysis indicates that PFS, ORR, and DCR were strongly
correlated with OS for GEC patients receiving TAs (r =0.85 for
PFS; r =0.86
for ORR; r =0.81
for DCR). No marked correlation was found between OS and CRs (r =0.43; P =0.18).
Conclusion: Although
the CR is a rate event in advanced GEC patients, adding the TAs to therapies,
especially for anti-EGFR agents, increases the chance of archiving CR in
comparison with the controls. PFS, ORR, and DCR are significantly correlated
with OS and could be used as surrogate endpoints in patients with GEC who have
received TA therapy, but not for CR.
Keywords: gastroesophageal
carcinoma, systematic review, novel molecular agents