110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

化疗对重症 COPD 非小细胞肺癌患者预后的影响
Authors Dong W, Du Y, Ma S
Received 1 August 2018
Accepted for publication 11 October 2018
Published 21 November 2018 Volume 2018:13 Pages 3805—3812
DOI https://doi.org/10.2147/COPD.S182173
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 3
Editor who approved publication: Professor Chunxue Bai
Background: The aim
of the study was to investigate if first-line chemotherapy improves total
survival time in non-small-cell lung cancer (NSCLC) patients complicated with
severe to very severe COPD.
Materials and methods: This
retrospective observational clinical study included 267 consecutive NSCLC
patients with COPD complications at the Department of Respiratory and Critical
Care Medicine of Tianjin Chest Hospital between January 2009 and January 2018.
Sixty-nine evaluable patients were included. The clinical characteristics,
toxicity profile, objective response rate, and prognosis were analyzed and
compared between patients receiving and those not receiving chemotherapy.
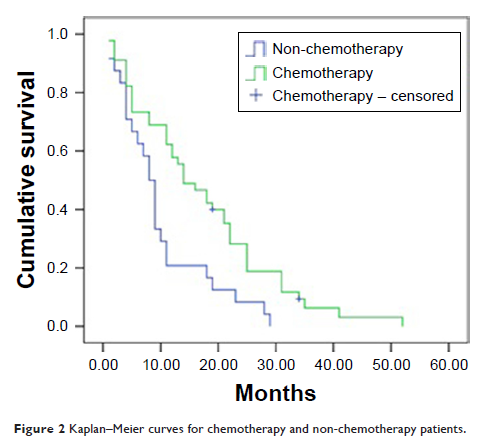
Results: Forty-five and
24 patients received first-line chemotherapy plus supportive care and
supportive care alone, respectively. Kaplan–Meier curves showed that patients
receiving chemotherapy had a statistically significant 6-month longer median
overall survival (OS) than that of patients receiving supportive care alone
(14.0, 95% CI: 8.5–19.5 vs 8.0, 95% CI: 6.4–9.6, respectively) (chi2=8.857, P =0.003). In the
multivariate Cox proportional hazard model adjusted for the most relevant
variables, the adjusted hazard ratio (HRadj) differed significantly for the
receipt of chemotherapy (HRadj=0.4464, 95% CI: 0.2495–0.7988; P =0.0066) but not
for gender (HRadj=0.8527, 95% CI: 0.4461–1.6298; P =0.6297), age
(HRadj=1.0021, 95% CI: 0.9609–1.0451; P =0.9214), histology (HRadj=1.4422, 95% CI:
0.6959–2.9889; P =0.3247), cancer stage (HRadj=1.9098, 95% CI:
0.8607–4.2375; P =0.1116), performance status score (HRadj=1.5155, 95%
CI: 0.7523–3.0529; P =0.2446), lung function (HRadj=1.3856, 95% CI: 0.7149–2.6857; P =0.3341), or
respiratory symptoms (HRadj=1.0518, 95% CI: 0.6032–1.8342; P =0.8586). Patients
with grade 3/4 adverse reactions accounted for 29% (13/45) of the chemotherapy
group.
Conclusion: The
results indicated that chemotherapy may improve the OS of NSCLC patients with
severe to very severe COPD.
Keywords: survival,
toxicity, first-line chemotherapy, GOLD grade