110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

骨外尤文氏肉瘤与骨骼尤文氏肉瘤患者的临床特征和结果比较: 3,178 个病例的 SEER 数据库分析
Authors Jiang S, Wang G, Chen J, Dong Y
Received 3 July 2018
Accepted for publication 12 October 2018
Published 23 November 2018 Volume 2018:10 Pages 6227—6236
DOI https://doi.org/10.2147/CMAR.S178979
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 3
Editor who approved publication: Dr Chien-Feng Li
Background: The
clinicopathological characteristics, outcomes and prognostic factors of primary
extraskeletal Ewing sarcoma (EES) remained insufficiently explored. We aimed to
examine these aspects and compared the same with skeletal Ewing sarcoma (SES).
Patients and methods: We identified
Ewing sarcoma, peripheral primitive neuroectodermal tumors or Askin tumor
patients who were registered in the Surveillance, Epidemiology, and End Results
database from 1973 to 2014. Clinicopathological features were assessed by using
Fisher’s exact tests. Cancer-specific survival (CSS) and overall survival (OS)
were estimated by using the Kaplan–Meier method and the Cox proportional
hazards model. Prognostic factors were identified by multivariate Cox
regression analysis.
Results: The age of
patients with EES was diagnosed to be higher and they were more likely to be
female (46.1% vs 36.2%; P <0.001), have tumor <10 cm (49.8% vs
35.4%; P <0.001),
have regional node involvement (5.4% vs 1.0%; P <0.001) and
receive surgery (69.1% vs 53.8%; P <0.001) compared to patients with skeletal tumors.
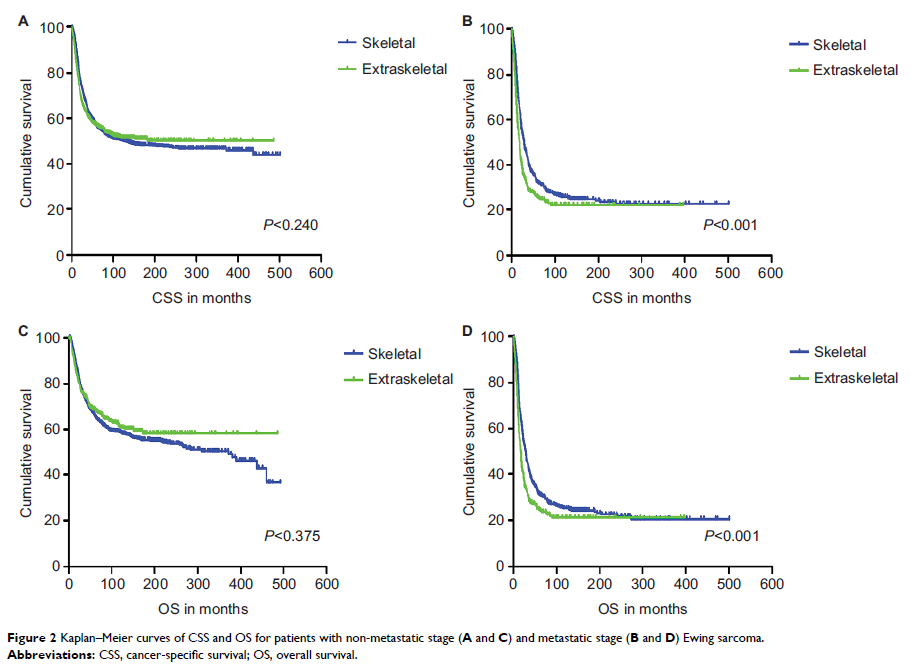
Metastatic status did not differ by origin. Kaplan–Meier analysis showed that
the origin had significant difference in CSS and OS among patients aged 0–19
years and with metastatic stage at presentation, but not in patients aged
20–39, ≥40 years and with no-metastatic stage. A Cox multivariable model
controlling for differences between groups confirmed inferior survival for
patients with EES. Age, tumor size, tumor stage and surgery were the most
important factors significantly influencing both CSS and OS in the EES and SES
patients. Race, year of diagnosis and tumor site were associated with CSS and
OS among patients with SES, but failed in EES.
Conclusion: The
clinicopathological characteristics, outcomes and prognostic factors differed
among patients with EES compared to patients with SES. Extraskeletal origin was
an unfavorable prognostic factor.
Keywords: Ewing
sarcoma, extraskeletal, skeletal, PNET, outcomes