110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

碳青霉烯类耐药鲍曼不动杆菌血流感染患者的危险因素和疗效回顾性比较分析:头孢哌酮钠舒巴坦钠耐药性及替加环素相关的死亡率增加
Authors Niu T, Xiao TT, Guo L, Yu W, Chen Y, Zheng B, Huang C, Yu X, Xiao Y
Received 27 March 2018
Accepted for publication 18 July 2018
Published 26 October 2018 Volume 2018:11 Pages 2021—2030
DOI https://doi.org/10.2147/IDR.S169432
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Eric Nulens
Background: Carbapenem-resistant Acinetobacter baumannii (CRAB) is a rapidly emerging, life-threatening nosocomial infection. This study aimed to explore the risk factors, clinical features, antimicrobial therapy, and outcomes of CRAB bloodstream infections (BSIs).
Methods: This is a retrospective, comparative analysis of data from patients with A. baumannii BSI, treated from 2012 to 2015 at a tertiary teaching hospital. Risk factors associated with CRAB BSI and factors associated with the 28-day mortality were evaluated using logistic analyses.
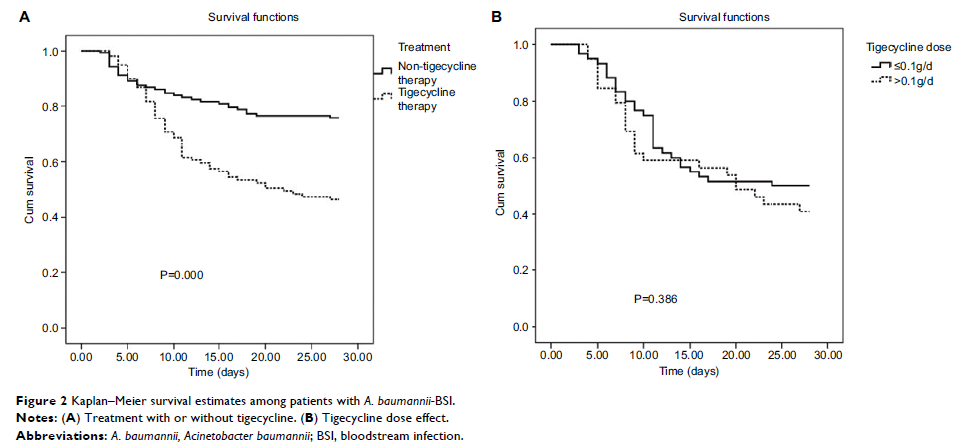
Results: Data from 293 patients with confirmed A. baumannii BSI were included; 242 (82.6%) patients had CRAB BSI and 51 (17.4%) patients had non-CRAB BSI. Risk factors significantly associated with CRAB BSI were a previous intensive care unit (ICU) stay (P =0.029), cefoperazone–sulbactam use (P =0.030), and carbapenem use (P =0.004). Among 236 patients with A. baumannii BSI who were evaluable at 28 days after receiving antibacterial therapy, there were 86 deaths. Factors associated with the 28-day mortality were ICU stay after BSI (P =0.040), readmission within 90 days (P =0.029), Acute Physiology and Chronic Health Evaluation II (APACHE II) score at diagnosis >19 (P =0.012), tigecycline therapy (P =0.021), presence of septic shock (P =0.029), and multiple organ failure (P =0.016). Death rates in patients treated with tigecycline were 53.5% vs 24.1% in patients treated with other agents. Among 186 patients with CRAB BSI evaluable at 28 days, 84 patients died. The associated risk factors were an ICU stay after BSI (P =0.036), APACHE II score >19 at diagnosis (P =0.002), presence of septic shock (P =0.030), and multiple organ failure (P =0.007).
Conclusion: This study demonstrated that an ICU stay and cefoperazone–sulbactam or carbapenem use were seen to be the risk factors associated with the development of CRAB BSI. Critical illness and tigecycline therapy were significantly associated with higher mortality of patients with A. baumannii BSI.
Keywords: Acinetobacter baumannii , carbapenem-resistant, bloodstream infection, cefoperazone–sulbactam, tigecycline