110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

TGF-β1 水平与接受放射疗法治疗的肺癌患者的淋巴细胞百分比相关
Authors Luo J, Hu S, Wei T, Sun J, Liu N, Wang J
Received 2 June 2018
Accepted for publication 11 September 2018
Published 26 November 2018 Volume 2018:11 Pages 8349—8355
DOI https://doi.org/10.2147/OTT.S175956
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 2
Editor who approved publication: Dr Yao Dai
Purpose: Plasma
TGF-β1 protein levels reportedly may predict the treatment outcomes of lung
cancer. We hypothesized that in patients with lung cancer treated with
radiation therapy (RT), TGF-β1 levels may correlate with the percentages of CD4+ T cells,
CD8+ T cells, and the CD4+/CD8+ T cell
ratio in peripheral blood.
Patients and methods: Eighty-two
lung cancer patients satisfied the inclusion criteria. Platelet-poor plasma was
obtained before RT, at the second and fourth weeks during RT, and at the end of
RT (pre-, during-, and post-RT, respectively). TGF-β1 was measured via ELISA,
while recording the percentages of lymphocyte subsets in peripheral blood.
Short-term efficacy was categorized as complete response, partial response,
stable disease, or progressive disease.
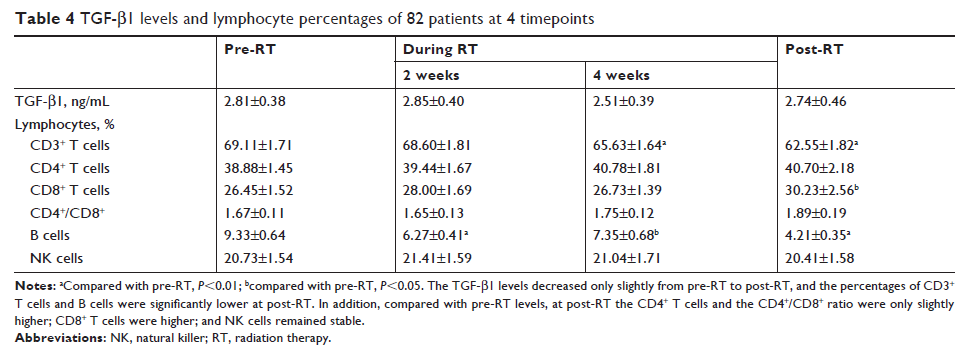
Results: Patients
who had significantly lower TGF-β1 protein levels after RT than pre-RT seemed
to have a better short-term effect (P <0.05) than those who had higher TGF-β1 levels.
There was a significant association between the TGF-β1 levels and percentages
of CD4+ T cells, CD8+ T cells,
or CD4+/CD8+ T cell
ratio during and at the end of RT. Changes in CD3+ T cells,
B cells, or natural killer cells were not statistically related to the changes
in TGF-β1 levels.
Conclusion: Lung
cancer patients with TGF-β1 levels in plasma after RT that are below pre-RT
levels may experience better short-term efficacy. The underlying mechanism may
be related to the influence of TGF-β1 on antitumor immunity.
Keywords: lung
cancer, radiotherapy, TGF-β1, lymphocytes, prognosis