110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

中国小儿侵袭性肺炎的肺炎球菌分离株的临床特征及耐药性分析
Authors Cai K, Wang Y, Guo Z, Xu X, Li H, Zhang Q
Received 14 August 2018
Accepted for publication 25 October 2018
Published 26 November 2018 Volume 2018:11 Pages 2461—2469
DOI https://doi.org/10.2147/IDR.S183916
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 3
Editor who approved publication: Dr Sahil Khanna
Purpose: Streptococcus pneumoniae causes
serious infections globally, including invasive pneumococcal disease (IPD). We
analyze clinical features of pediatric IPD cases identified in China and
antibiotic susceptibility of isolated pneumococcal strains.
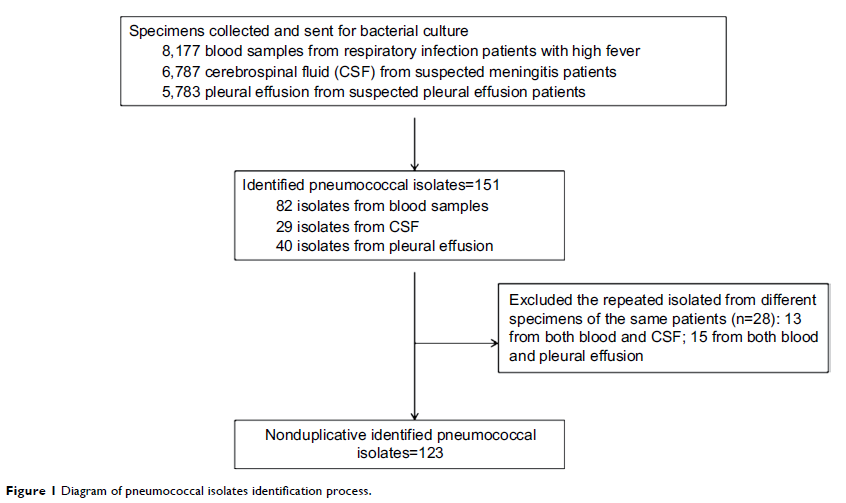
Methods: Confirmed
pediatric IPD patients were prospectively recruited to the study. Symptoms at
the time of hospitalization, laboratory tests, antimicrobial susceptibility of
pneumococcal isolates, treatments, hospital stay, and residual findings at
discharge were analyzed systematically.
Results: From
January 2008 to December 2017, a total of 123 hospitalized children diagnosed
with IPD were enrolled: 68 from pediatric departments of Xinhua Hospital, and
55 from Lanzhou University Second Hospital. Of these pediatric IPD patients, 81
(65.86%) were male, and 98 (79.67%) <5 years old. Most cases (96, 78.05%)
were diagnosed during the cold season between September and February. Sepsis
was observed in 82 (66.67%) patients, 48 (39.02%) children were diagnosed with
meningitis, 41 (33.33%) with pneumonia, 30 (24.39%) with pleurisy, and 4
(3.25%) with osteomyelitis. Underlying diseases were noted in 35 (28.45%)
patients and concurrent infections in 45 (36.58%). The overall mortality rate
was 2.44%. IPD children who developed sepsis and necrotizing pneumonia showed
higher proportions of intensive care-unit admission, intravenous γ-globulin,
glucocorticoid use, hemofiltration and ventilator, and longer duration of
fever, hospital stay, and antibiotic use than nonsepsis and pneumonia subjects.
Antimicrobial resistance of S. pneumoniae showed a highly unsusceptible rate for
erythromycin (96.75%), trimethoprim-sulfamethoxazole (79.67%), and tetracycline
(77.23%). All isolates were sensitive to vancomycin, linezolid, and
levofloxacin.
Conclusion: Clinical
symptoms were severe in the majority of pediatric IPD patients. More intensive
treatments were demanded for IPD children with sepsis and necrotizing
pneumonia. High resistance rates for erythromycin,
trimethoprim–sulfamethoxazole, and tetracycline were found.
Keywords: Streptococcus pneumoniae ,
children, invasive pneumococcal disease, antimicrobial resistance