110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

肿瘤免疫背景中免疫检查点的编排及其在食管鳞状细胞癌中的预后意义
Authors Zhao JJ, Zhou ZQ, Wang P, Chen CL, Liu Y, Pan QZ, Zhu Q, Tang Y, Weng DS, Xia JC
Received 30 July 2018
Accepted for publication 30 October 2018
Published 28 November 2018 Volume 2018:10 Pages 6457—6468
DOI https://doi.org/10.2147/CMAR.S181949
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 4
Editor who approved publication: Dr Xueqiong Zhu
Introduction: Esophageal
squamous cell carcinoma (ESCC) develops in a background of chronic
inflammation; therefore, it is a promising candidate for treatment by
immunotherapy. Although tumor immunity is critically involved in tumor growth
and metastasis in ESCC, important gaps exist in our understanding of its immune
microenvironment. This study aimed to investigate the expression and prognostic
significance of immune checkpoint proteins in ESCC and the associated T-cell
densities.
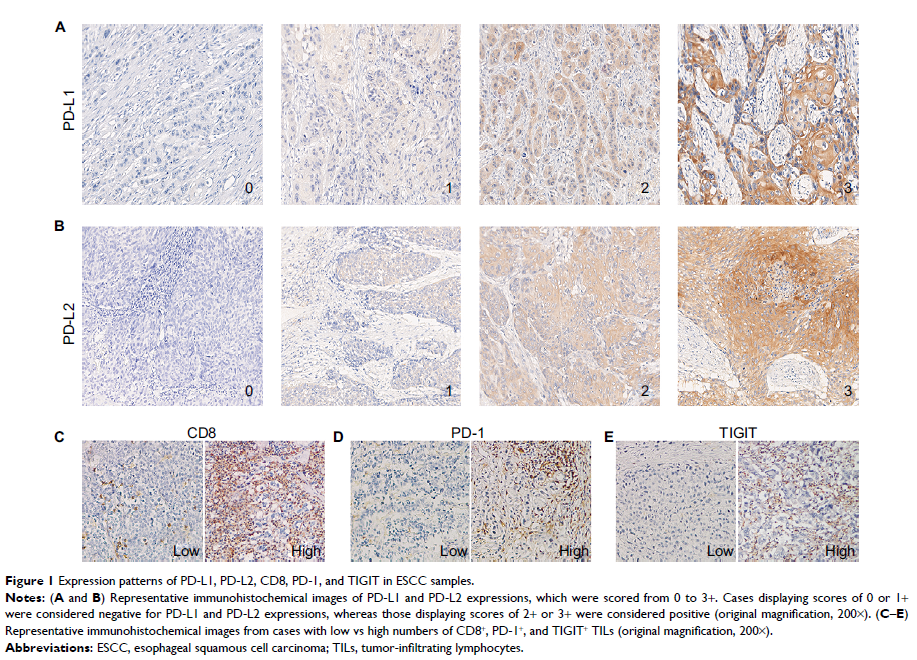
Materials and methods: We
investigated the infiltration of CD8+ T cells and the expressions of immune
checkpoint proteins (PD-1, TIGIT, PD-L1, and PD-L2) in 154 primary ESCC
patients by immunohistochemistry. The correlation of immune checkpoint
proteins’ expression and clinical outcomes was determined by Kaplan–Meier test
and multivariate Cox regression analysis.
Results: PD-L1 and PD-L2
expression were detected in 45.5 and 59.7% of the ESCC samples, respectively.
The high densities of PD-1+ and TIGIT+ tumor-infiltrating
lymphocytes (TILs) were expressed in 47.4 and 49.4% of the ESCC patients,
respectively. The number of PD-1+ TILs was significantly positively correlated
with CD8+ TILs (P <0.001).
Cases displaying high PD-L1 expression exhibited consistently high CD8+ T-cell
infiltration (P =0.0157).
Increased numbers of PD-1+ and TIGIT+ TILs alone or both, as well as PD-L1 and
PD-L2 expression alone or both, were significantly and associated with a
shorter overall survival among these patients. The combined analysis of the
expression of PD-1, TIGIT, PD-L1, and PD-L2 found that a group of patients with
PD-1+/TIGIT+ TILs and
PD-L1- and/or PD-L2-positive tumor cells had the worst prognosis in primary
ESCC.
Conclusion: These immune
profiles of checkpoint proteins expression should guide the selection of ESCC
patients to receive suitable immunotherapies.
Keywords: biomarker,
PD-1, prognostic significance, immune microenvironment, tumor-infiltrating
lymphocytes