110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

CCBE1 在结直肠癌中表达的临床意义
Authors Zhao YR, Liu H, Xiao LM, Jin CG, Zhang ZP, Yang CG
Received 28 July 2018
Accepted for publication 24 September 2018
Published 30 November 2018 Volume 2018:10 Pages 6581—6590
DOI https://doi.org/10.2147/CMAR.S181770
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Justinn Cochran
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Purpose: The
identification and discovery of prognostic markers for colorectal cancer (CRC)
are of great clinical significance. CCBE1 is expressed in various tumors and
its expression correlates with lymphangiogenesis and angiogenesis. However, the
association between CCBE1 expression and CRC outcome has not been reported. The
aim of this study was to investigate clinical significance of CCBE1 expression
in CRC.
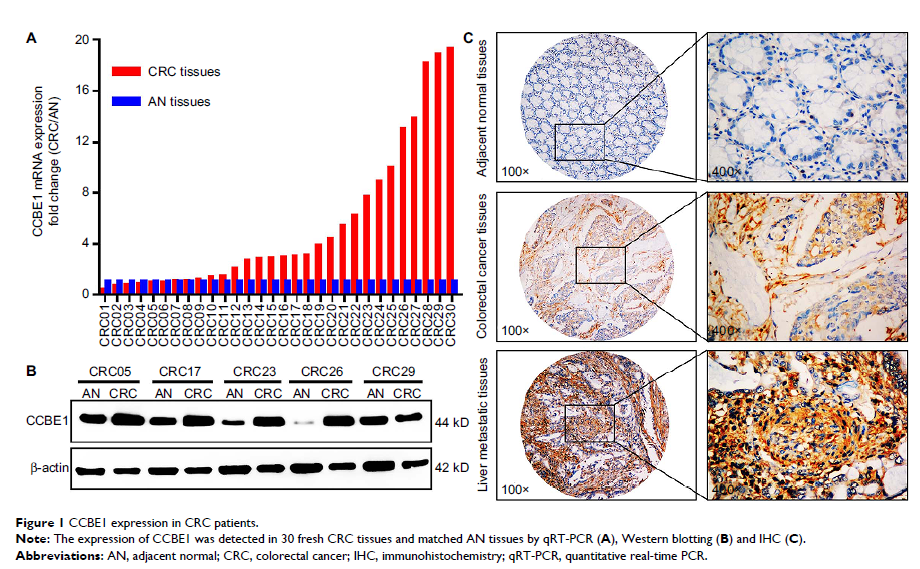
Patients and methods: CCBE1
expression was examined in 30 pairs of fresh CRC tissues and compared with
adjacent normal (AN) tissues using quantitative real-time PCR (qRT-PCR),
Western blotting and immunohistochemistry (IHC) staining. Tissue microarray
immunohistochemical staining was used to study the CCBE1 expression
characteristics of 204 CRC patient samples collected from January 2002 to
December 2007, and the relationship of CCBE1 with clinicopathological features
and prognosis of CRC was analyzed.
Results: CCBE1 was
highly expressed in CRC tissues compared with matched AN tissues (P =0.001). Moreover,
high expression of CCBE1 was significantly associated with tumor
differentiation, lymph node metastasis, vascular invasion, liver metastasis and
TNM stage in CRC patients (P ≤0.01). Kaplan–Meier survival analysis revealed that
high CCBE1 expression, poor tumor differentiation, lymph node metastasis and vascular
invasion were significantly associated (all P <0.001) with
poor prognosis for patients. Furthermore, univariate and multivariate Cox
analysis revealed that high CCBE1 expression, poor tumor differentiation, lymph
node metastasis and vascular invasion were independent risk factors for both
overall survival (OS) and disease-free survival (DFS) of CRC patients
(all P <0.05).
OS and DFS of 267 CRC patients from The Cancer Genome Atlas (TCGA) database
showed the same trend (log-rank P =6e-04, HR [high] =2.4; log-rank P =0.0081, HR [high]
=1.9).
Conclusion: High levels of
CCBE1 contribute to the aggressiveness and poor prognosis of CRC. CCBE1 can
serve as a novel potential biomarker to predict CRC patients’ prognosis.
Keywords: CCBE1,
prognosis, colorectal cancer, CRC, survival analysis, TCGA