110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

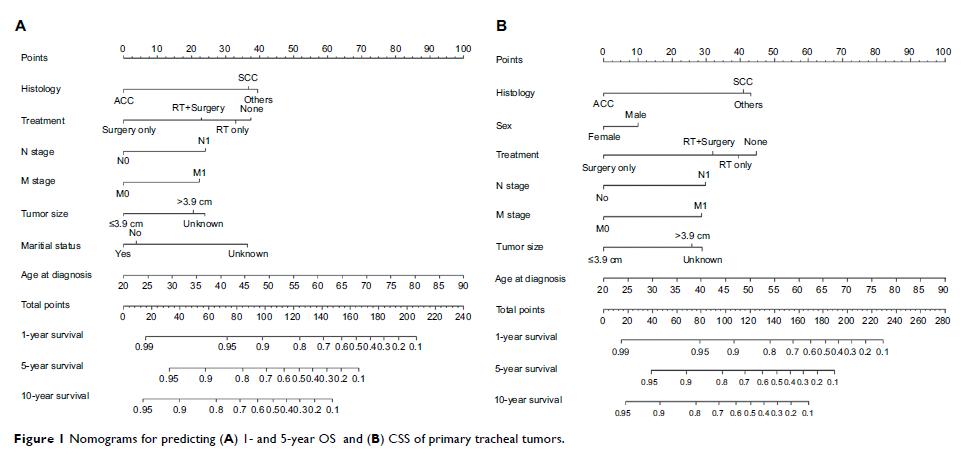
用于预测原发性气管肿瘤患者生存结果的诺模图:一项大型以人群为基础的分析
Authors Wen J, Liu D, Xu X, Chen D, Chen Y, Sun L, Chen J, Fan M
Received 5 September 2018
Accepted for publication 16 November 2018
Published 11 December 2018 Volume 2018:10 Pages 6843—6856
DOI https://doi.org/10.2147/CMAR.S186546
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 2
Editor who approved publication: Dr Rituraj Purohit
Background: The aim
of this study was to develop and validate reliable nomograms to predict
individual overall survival (OS) and cancer-specific survival (CSS) for
patients with primary tracheal tumors and further estimate the role of
postoperative radiotherapy (PORT) for these entities.
Patients and methods: A total of 405
eligible patients diagnosed between 1988 and 2015 were selected from the
Surveillance, Epidemiology, and End Results database. All of them were randomly
divided into training (n=303) and validation (n=102) sets. For the purpose of
establishing nomograms, the Akaike information criterion was employed to select
significant prognostic factors in multivariate Cox regression models. Both
internal and external validations of the nomograms were evaluated by Harrell’s
concordance index (C-index) and calibration plots. Propensity score matching
(PSM) method was performed to reduce the influence of selection bias between
the PORT group and the non-PORT group.
Results: Two
nomograms shared common variables including age at diagnosis, histology, N and
M stages, tumor size, and treatment types, while gender was only incorporated
in the CSS nomogram. The C-indices of OS and CSS nomograms were 0.817 and
0.813, displaying considerable predictive accuracy. The calibration curves indicated
consistency between the nomograms and the actual observations. When the
nomograms were applied to the validation set, the results remained
reconcilable. Moreover, the nomograms showed superiority over the
Bhattacharyya’s staging system with regard to the C-indices. After PSM, PORT
was not associated with significantly better OS or CSS. Only squamous cell
carcinoma (SCC) patients in the PORT group had improved OS compared to non-PORT
group.
Conclusion: The first
two nomograms for predicting survival in patients with primary tracheal tumors
were proposed in the present study. PORT seems to improve the prognosis of SCC
patients, which needs further exploration.
Keywords: nomogram,
primary tracheal tumors, overall survival, cancer-specific survival, propensity
score matching analysis