110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

被切除的淋巴结的数量与 T2N0 非小细胞肺癌患者的长期存活率相关
Authors Wen YS, Xi KX, Xi KX, Zhang RS, Wang GM, Huang ZR, Zhang LJ
Received 1 September 2018
Accepted for publication 12 November 2018
Published 12 December 2018 Volume 2018:10 Pages 6869—6877
DOI https://doi.org/10.2147/CMAR.S186047
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
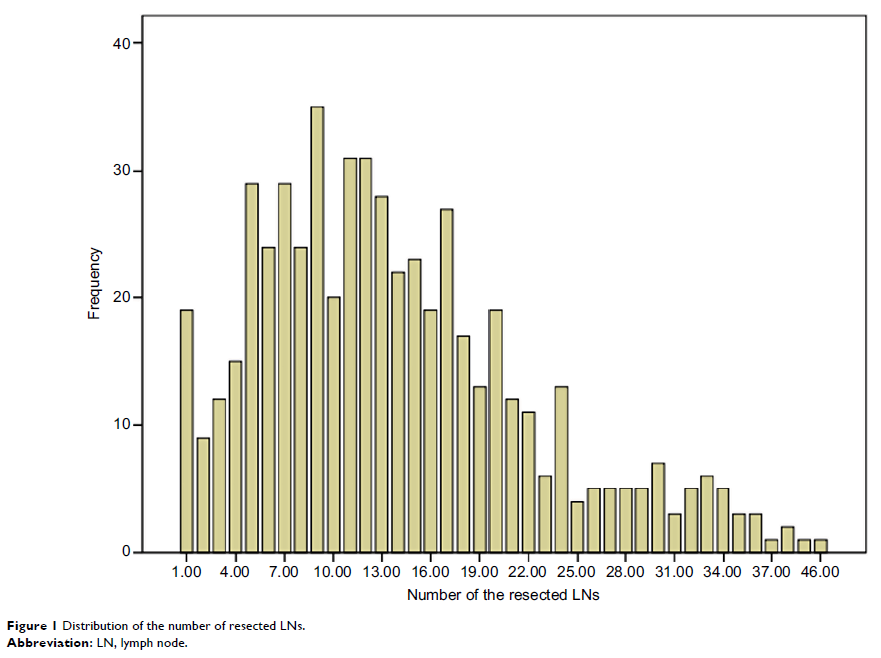
Objective: For the
patients with pathologic T2 N0 non-small cell lung cancer (NSCLC), the extent
of lymph node (LN) removal required for survival is controversial. We aimed to
explore the prognostic significance of examined LNs and to identify how many
nodes should be examined.
Methods: We
reviewed 549 patients who underwent pulmonary or pneumonectomy surgery or plus
lymphadenectomy who were confirmed as T2 stage and LN negative by postoperative
pathological diagnosis. According to Martingale residuals of the Cox model, the
patients were classified into four groups by the number of examined LNs (1–2
LNs, 3–7 LNs, 8–11 LNs, and ≥12 LNs). Kaplan–Meier analysis and Cox regression
analysis were used to evaluate the association between survival and the number
of examined LNs.
Result: Compared
with the 1–2 LNs, 3–7 LNs, and 8–11 LNs groups, the survival was significantly
better in the ≥12 LNs group. The 5-year cancer-specific survival rate was 60.5%
for patients with 1–2 negative LNs, compared with 68.7%, 72.6%, and 78.4% for
those with 3–7, 8–11, and >11 LNs examined, respectively. The 7-year
cancer-specific survival rate was 52.9% for patients with 1–2 negative LNs,
compared with 63.7%, 63.8%, and 70.8% for those with 3–7, 8–11, and >11 LNs
examined, respectively (P =0.045). There was a significant drop in mortality
risk with the examination of more LNs. The lowest mortality risk occurred in
those with 32 or more LNs examined. Multivariate analysis showed that age and
the number of examined LNs were strong independent predictors of survival.
Conclusion: The
number of examined LNs is a strong independent prognostic factor. Our study
demonstrates that patients with T2 N0 NSCLC should have at least 12 LNs
examined and that the results of this study may provide information for the
optimal number of resected LNs in surgery.
Keywords: number of
resected lymph nodes, non-small cell lung cancer, survival outcome