110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

小儿肝移植后遵守医疗方案:一个系统评价和荟萃分析
Authors Meng X, Gao W, Wang K, Han C, Zhang W, Sun C
Received 23 July 2018
Accepted for publication 23 November 2018
Published 17 December 2018 Volume 2019:13 Pages 1—8
DOI https://doi.org/10.2147/PPA.S181195
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Purpose: Adherence to
the medical regimen after pediatric liver transplantation is crucial for good
clinical outcomes. However, the existing literature provides inconsistent
evidence regarding the prevalence of and risk factors for nonadherence to the
medical regimen after pediatric liver transplantation. This study aimed to
investigate such nonadherence after pediatric liver transplantation and risk
factors associated with this nonadherence using findings of reported studies.
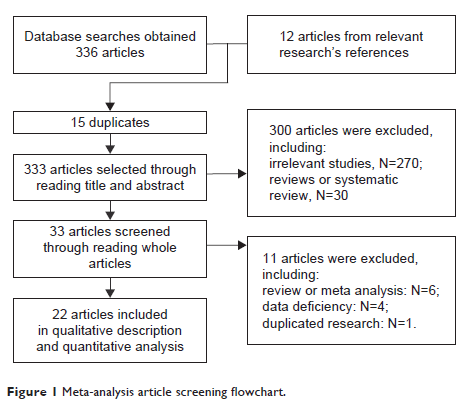
Methods: The electronic
databases of Excerpta Medica, Ovid Technologies, PubMed and WanFang Data were
searched using the keywords “adherence”, “liver transplant” and “paediatric”.
Additionally, relevant references cited in related studies were used to obtain
original articles. Using 22 original articles, data regarding nonadherence to
the medical regimen after pediatric liver transplantation were quantitatively
combined, and risk factors associated with nonadherence were qualitatively identified.
Average rates of nonadherence in four areas of medical regimens were
calculated. The heterogeneity of the included original articles was also
analyzed. When I 2>50 and P <0.05, a random
effects model was used; otherwise, a fixed effects model was used. Moreover,
Egger’s and Begg’s tests were used to evaluate publication bias, if any, and
original articles with P >0.05 were considered to have no publication bias.
Results: The clinical
attendance nonadherence rate was 45% (95% confidence interval [CI]: 39–51),
global nonadherence rate was 17% (95% CI: 13–21) and immunosuppression
nonadherence rates were 39% (95% CI: 26–52) and 34% (95% CI: 30–39) for
cyclosporine and tacrolimus, respectively. Risk factors included older age of
the pediatric patient, low family cohesion, poor social functioning, poor
mental health and single-parent family.
Conclusions: The
nonadherence rate in pediatric liver transplantation is high. Therefore,
intervention on the basis of risk factors, such as mental health and family function,
may be necessary. Moreover, a standard technique for assessing nonadherence to
the medical regimen after pediatric liver transplantation, comprising as many
dimensions as possible, is required in order to be more objective and
comprehensive when assessing nonadherence.
Keywords: compliance,
transplant, pediatrics, hepar, hepatic