110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

胸腔镜联合腹腔镜食管癌切除术后镇痛:连续输注和硬膜外间歇性推注胸部给药方案的随机对照
Authors Wei K, Min S, Hao Y, Ran W, Lv F
Received 24 September 2018
Accepted for publication 27 November 2018
Published 18 December 2018 Volume 2019:12 Pages 29—37
DOI https://doi.org/10.2147/JPR.S188568
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 2
Editor who approved publication: Dr Katherine Hanlon
Purpose: Judicious
postoperative pain management after thoracoscopic–laparoscopic esophagectomy
(TLE) facilitates enhanced rehabilitation. Thoracic epidural analgesia (TEA)
offers many benefits in esophagectomy, while several complications are
associated with the delivery mode by continuous epidural infusion. This study
compared the efficiency and safety of intermittent epidural bolus to continuous
epidural infusion for pain management after TLE.
Patients and methods: Sixty patients,
aged 18–80 years, with American Society of Anesthesiologists classes I–III and
scheduled for TLE with combined general anesthesia and TEA were randomly
allocated to two groups. Patients received either a continuous epidural
infusion with 0.3% ropivacaine and 1.5 µg/mL fentanyl at 6 mL/h plus a
patient-controlled bolus of 3 mL (continuous group) or an intermittent bolus of
6 mL of the same solution on demand with lockout time of 30 minutes
(intermittent group). If the patient complained of pain and the visual analog
scale score was >4, an intravenous injection of tramadol or dezocine was
administered as rescue treatment. The primary outcome variable was the consumption
of epidural opioids and local anesthetics for TEA.
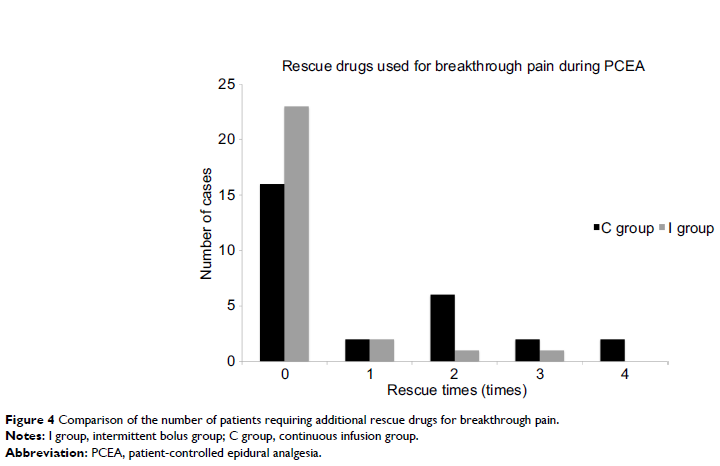
Results: TEA for pain
management following TLE by intermittent epidural bolus was associated with
significantly lower consumption of fentanyl and ropivacaine and lower
incidences of breakthrough pain and hypotension than continuous epidural
infusion. No significant differences were observed between the two groups in
terms of pain score at rest or while coughing, patient satisfaction, or
incidence of postoperative complications.
Conclusion: Compared with
continuous epidural infusion, TEA by on-demand intermittent bolus greatly
reduced the consumption of local anesthetics and opioids with comparable pain
relief and little impairment in hemodynamics when used for pain management
after TLE.
Keywords: thoracic
epidural analgesia, thoracoscopic–laparoscopic esophagectomy, postoperative
pain