110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

Cytokine production capabilities of human primary monocyte-derived macrophages from patients with diabetes mellitus type 2 with and without diabetic peripheral neuropathy
Authors Alvarado-Vázquez PA, Grosick RL, Moracho-Vilrriales C, Ward E, Threatt T, Romero-Sandoval EA
Received 4 September 2018
Accepted for publication 15 November 2018
Published 19 December 2018 Volume 2019:12 Pages 69—81
DOI https://doi.org/10.2147/JPR.S186372
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 3
Editor who approved publication: Dr Michael Schatman
Introduction: Monocytes from
patients with diabetes mellitus type 2 (DM2) are dysfunctional, persistently
primed, and prone to a proinflammatory phenotype. This may alter the phenotype
of their differentiation to macrophages and result in diabetic peripheral
neuropathy (DPN), nerve damage, nerve sensitization, and chronic pain. We have
previously demonstrated that CD163 is a molecule that promotes an
anti-inflammatory cellular phenotype in human primary macrophages, but this has
not been proven in macrophages from patients with DM2 or DPN. Thus, we
hypothesize that macrophages from patients with DM2 or DPN display an altered
proinflammatory functional phenotype related to cytokine production and that
the induction of CD163 expression will promote a more homeostatic phenotype by
reducing their proinflammatory responsiveness.
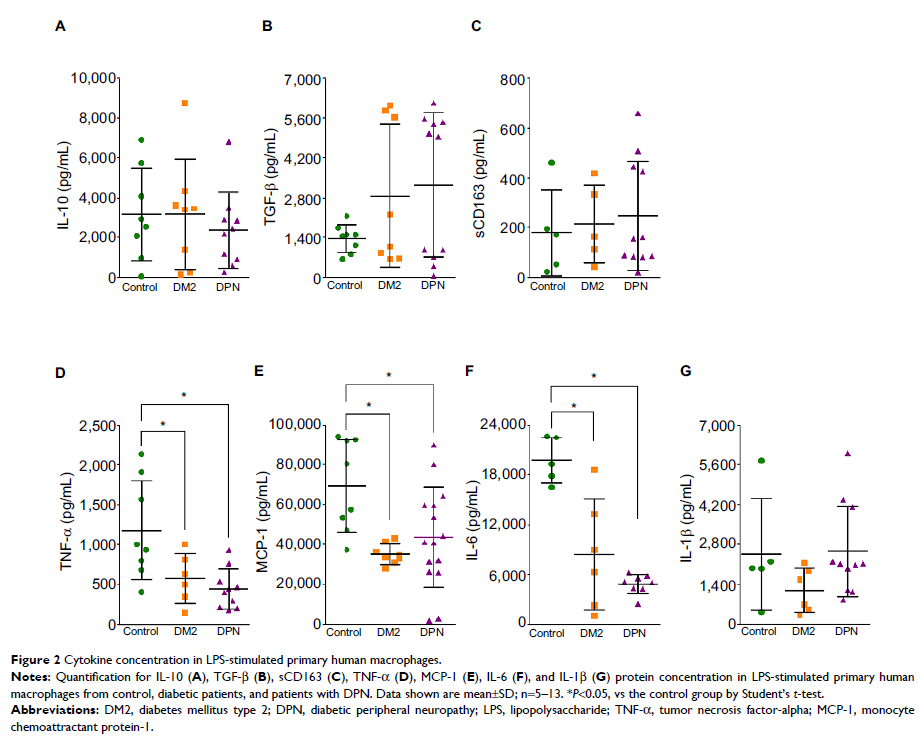
Patients and methods: We tested these
hypotheses in vitro using blood monocyte-derived macrophages from healthy
subjects and patients with DM2 with and without DPN. Cells were incubated in
the presence or the absence of 5 µg/mL of lipopolysaccharide (LPS). The
concentrations of interleukin-10, interleukin-6, tumor necrosis factor-alpha
(TNF-α), TGF-β, and monocyte chemoattractant protein-1 (MCP-1) were measured
using ELISA assays. Macrophages were transfected with an empty vector plasmid
or a plasmid containing the CD163 gene using mannosylated polyethylenimine
nanoparticles.
Results: Our results
show that nonstimulated DM2 or DPN macrophages have a constitutive primed
proinflammatory state and display a deficient production of proinflammatory
cytokines upon a proinflammatory challenge when compared to healthy
macrophages. CD163 induction produced an anti-inflammatory phenotype in the
healthy control group, and this effect was partial in DM2 or DPN macrophages.
Conclusion: Our results
suggest that diabetic macrophages adopt a complex phenotype that is only
partially reversed by CD163 induction. Future experiments are focused on
elucidating this differential responsiveness between healthy and diabetic
macrophages.
Keywords: primary
human macrophages, CD163, transfection, LPS