110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

通过靶向 Bcl-2 逆转卵巢癌多细胞球体中的铂抗性
Authors Yang Y, Li S, Sun Y, Zhang D, Zhao Z, Liu L
Received 24 September 2018
Accepted for publication 1 January 2019
Published 29 January 2019 Volume 2019:12 Pages 897—906
DOI https://doi.org/10.2147/OTT.S187015
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 3
Editor who approved publication: Dr Takuya Aoki
Purpose: Peritoneal
metastasis is the most common pathway for the spread of ovarian cancer. Ovarian
cancer cells in ascites prefer to aggregate into the more chemoresistant
multicellular spheroids (MCSs), leading to treatment failure and disease
recurrence. We previously established a suspension MCS model of ovarian cancer
cells in vitro and found that the MCS cells acquired drug resistance to
cisplatin. In the present study, we aimed to uncover the underlying mechanism
of the platinum resistance of MCS and the potential targets to reverse the drug
resistance.
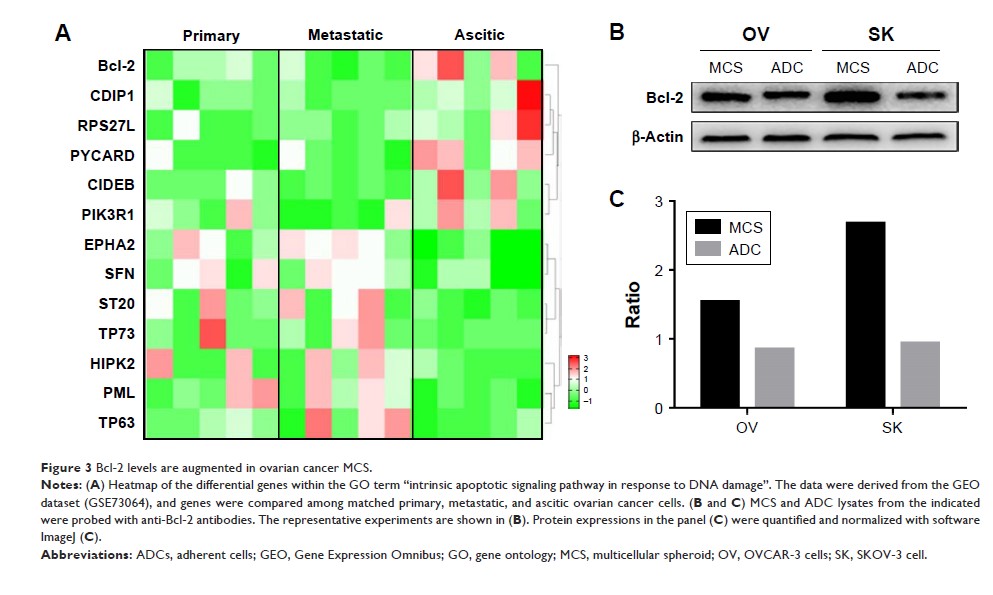
Materials and methods: MCS
models were established for the phenotypic studies, including proliferation,
invasion, migration, drug resistance, apoptosis assays, and signaling pathway
analysis. The key molecule, Bcl-2, was screened by profile analysis and
validated by Western blotting. siRNA was used to verify the
anti-cisplatin-induced apoptosis effect of Bcl-2. The Bcl-2 inhibitor, ABT-737,
was used for improving the sensitivity of MCS to cisplatin. The 50% inhibitory
concentrations (IC50) were measured by viability assays treated with different
concentrations of cisplatin. Flow cytometry and Western blotting were used for
quantification of drug-induced apoptosis.
Results: The
ovarian cancer MCS showed a proliferation-stagnant but invasive phenotype when
resuspended. When treated with cisplatin, MCS cells showed much higher
viability, with significantly fewer apoptotic cells than the adherent cells.
Levels of Bcl-2 were upregulated in ovarian cancer ascitic cells and MCS cells.
Bcl-2 knockdown by siRNA or blockage by ABT-737 enhanced the cisplatin-induced
apoptosis and reduced the 50% inhibitory concentrations of cisplatin for MCS by
58.5% and 88.2%, respectively.
Conclusion: The
upregulated Bcl-2 contributes to cisplatin resistance in our MCS model and
targeting it sensitizes the MCS to cisplatin treatment. This provides us a
preliminary treatment method for ovarian cancer peritoneal metastasis.
Keywords: Bcl-2,
drug resistance, molecular targeted therapy, multicellular spheroids, ovarian
neoplasms