111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

同时使用 EGFR-TKI 和全脑放疗与单纯应用 EGFR-TKI 作为晚期 EGFR 突变的非小细胞肺癌脑转移的一线治疗的疗效比较:一个回顾性队列研究
Authors He ZY, Li MF, Lin JH, Lin D, Lin RJ
Received 22 August 2018
Accepted for publication 1 February 2019
Published 14 March 2019 Volume 2019:11 Pages 2129—2138
DOI https://doi.org/10.2147/CMAR.S184922
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 2
Editor who approved publication: Dr Beicheng Sun
Background: Non-small-cell lung cancer (NSCLC) is a
global public health problem, and brain is a common metastatic site in advanced
NSCLC. Currently, whole-brain radiotherapy (WBRT) remains a major treatment for
brain metastases, while EGFR-tyrosine kinase inhibitor (TKI) is the standard
treatment for advanced NSCLC harboring EGFR mutations, which is also effective for brain
metastases. However, whether EGFR-TKIs plus radiotherapy is superior to
EGFR-TKIs alone for the treatment of advanced EGFR -mutant NSCLS
with brain metastases remains controversial. This study aimed to compare the
efficacy of concurrent EGFR-TKIs and WBRT vs EGFR-TKI alone in a retrospective
cohort of advanced EGFR -mutant NSCLS with brain metastases.
Patients and methods: The medical records of 104 treatment-naïve, advanced EGFR -mutant NSCLC
patients with brain metastases were retrospectively reviewed, and there were 56
patients undergoing concurrent EGFR-TKI and WBRT, and 48 patients given
EGFR-TKI alone, including 20 cases with salvage WBRT upon brain metastasis
progression. The survival prognosis was compared between the two cohorts.
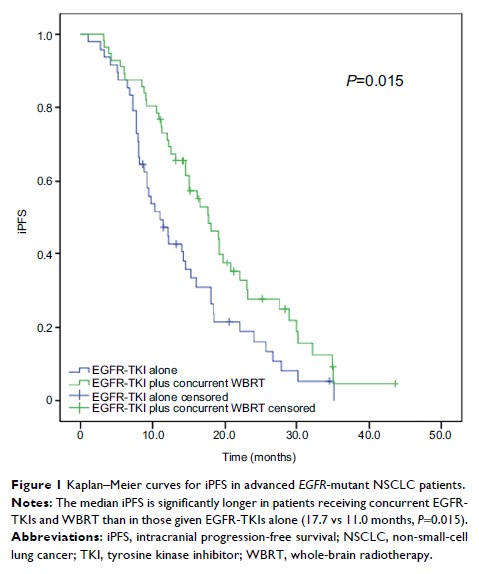
Results: The
baseline clinicopathologic factors were balanced between the two cohorts. After
a median follow-up of 23 months, 35.6% of the study subjects survived.
Concurrent EGFR-TKI and WBRT significantly improved the median intracranial PFS
(iPFS) compared with EGFR-TKI alone (17.7 vs 11.0 months, P =0.015); however,
no significant difference was seen in median overall survival between the two
cohorts (28.1 vs 24.0 months, P =0.756). In addition, the median iPFS was found to
significantly vary in the number of brain metastases (≤3 vs>3 metastases:
18.0 vs 12.5 months, P =0.044). Subgroup analysis showed that concurrent
EGFR-TKI and WBRT improved median iPFS compared with EGFR-TKI alone in patients
with more than three brain metastases (P =0.001); however, no significant difference was
observed between the two regimens in patients with three or less brain
metastases (P =0.526).
Conclusion: Our
data demonstrate that concurrent EGFR-TKI and WBRT achieves longer iPFS than
EGFR-TKI alone in advanced EGFR -mutant NSCLC with brain metastases. In
advanced EGFR -mutant
NSCLC with three or less brain metastases, EGFR-TKI alone may be an option as a
first-line therapy.
Keywords: non-small-cell
lung cancer, brain metastasis, epidermal growth factor receptor, tyrosine
kinase inhibitor, whole-brain radiotherapy