111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

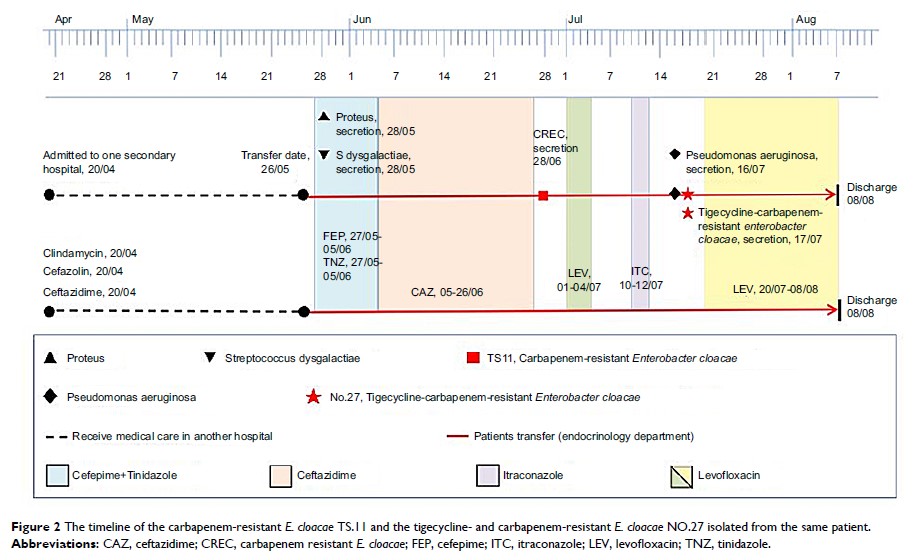
替加环素和碳青霉烯类耐药的阴沟肠杆菌感染的危险因素
Authors Jiang Y, Jia X, Xia Y
Received 11 October 2018
Accepted for publication 31 January 2019
Published 20 March 2019 Volume 2019:12 Pages 667—674
DOI https://doi.org/10.2147/IDR.S189941
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Background: Tigecycline
is regarded as a last resort treatment for carbapenem-resistant Enterobacter cloacae (CREC)
infections, and increasing numbers of tigecycline- and
carbapenem-resistant E. cloacae (TCREC) isolates have been reported in
recent years. However, risk factors and clinical impacts of these isolates are
poorly characterized.
Patients and methods: We
conducted a retrospective case-case-control study of hospitalized patients with
TCREC infection during the period 2012–2016 in Chongqing, China. Case patients
with TCREC and those with CREC were compared to a control group with no E. cloacae infection.
Multivariate logistic regression models were used to identify independent risk
factors for acquiring TCREC and CREC.
Results: A total
of 36 TCREC cases, 36 CREC cases, and 100 controls were enrolled in our study.
Multivariable analysis indicated that nasal catheter (OR: 8.9; 95% CI:
1.1–75.2), exposure to penicillin (OR: 95.9; 95% CI: 8.9–1038.3),
aminoglycosides (OR: 42.1; 95% CI: 2.1–830.6), and fluoroquinolones (OR: 18.6;
95% CI: 1.9–185.6) were independent predictors for acquiring TCREC. In
addition, venous catheterization (OR: 12.2; 95% CI: 2.5–58.5), penicillin (OR:
30.8; 95% CI: 7.9–120.0), and broad-spectrum cephalosporin (OR: 5.0; 95% CI: 1.5–17.3)
were independently associated with CREC acquisition.
Conclusion: Reasonable
antibiotic stewardship programs and surveillance are necessary to control the
tigecycline resistance among high-risk patients.
Keywords: carbapenem
resistance, tigecycline, Enterobacter cloacae , risk factor