111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

原发肿瘤位置是肺腺癌存活的重要预测因子
Authors Wang Z, Li M, Teng F, Kong L, Yu J
Received 30 October 2018
Accepted for publication 11 February 2019
Published 21 March 2019 Volume 2019:11 Pages 2269—2280
DOI https://doi.org/10.2147/CMAR.S192828
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Andrew Yee
Peer reviewer comments 2
Editor who approved publication: Dr Beicheng Sun
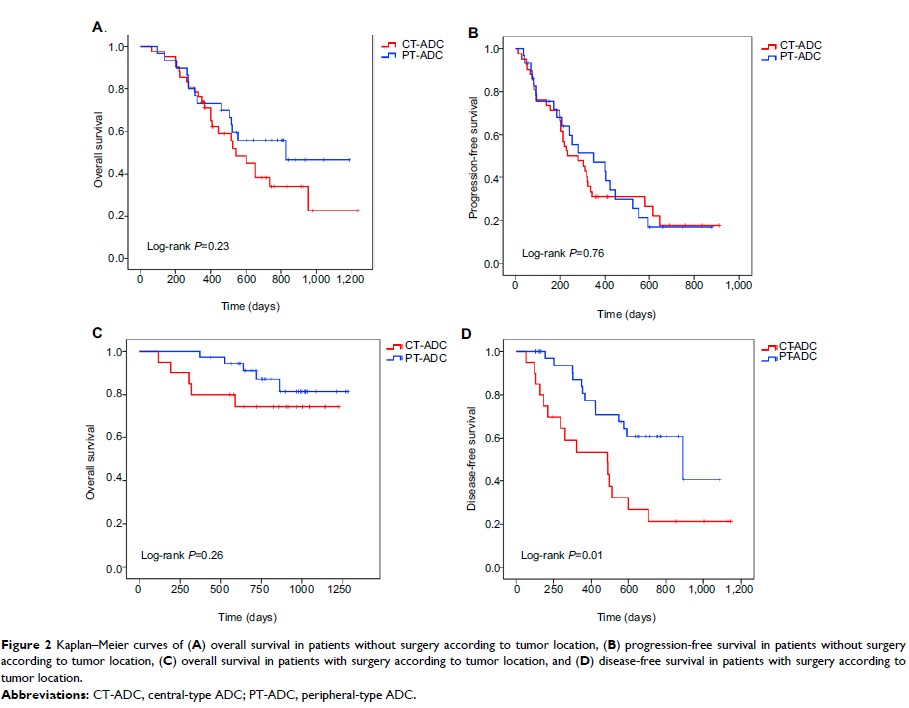
Purpose: The
prognostic value of tumor location in pulmonary adenocarcinoma (ADC) is
controversial. We compared the prognosis and relevant data between central-type
ADC (CT-ADC) and peripheral-type ADC (PT-ADC) in order to identify the reasons
for the different outcomes between them and to improve the treatment strategy
and prognosis of these two types.
Patients and methods: Data of
256 patients with pathologically diagnosed ADC were retrospectively reviewed.
The prognostic factors for disease-free survival (DFS), progression-free
survival (PFS), and overall survival (OS) were analyzed using univariate and
multivariate analyses.
Results: A total
of 124 and 132 patients had CT-ADC and PT-ADC, respectively. CT-ADC was
associated with an earlier age, poorer Karnofsky Performance Status (KPS),
higher rates of advanced stage, bone metastasis, contralateral pulmonary
metastasis, and pleural effusion. Besides, CT-ADC showed a trend toward lower
rate of EGFR mutation. Patients with CT-ADC had a significantly shorter PFS/DFS
and OS than did those with PT-ADC. Multivariate analysis revealed that advanced
stage, central-type location, EGFR wild-type, no surgery, presence of COPD, and
interstitial lung disease (ILD) were independent poor prognostic factors for
OS. The rate of surgery was significantly lower in patients with CT-ADC. Among
patients with ILD or COPD, OS is shorter in patients with central- than
peripheral-type tumors.
Conclusion: CT-ADC is
associated with poorer survival than PT-ADC and the lower rate of surgery in
patients with CT-ADC is an important reason for this. Tumor location of
pulmonary ADC plays a critical role in predicting prognosis and choosing
therapeutic strategies.
Keywords: lung
cancer, EGFR, surgery, clinical stage, comorbidity