111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

环丝氨酸治疗多药耐药性结核病:中国的一项回顾性队列研究
Authors Li Y, Wang F, Wu L, Zhu M, He G, Chen X, Sun F, Liu Q, Wang X, Zhang W
Received 22 November 2018
Accepted for publication 3 January 2019
Published 29 March 2019 Volume 2019:12 Pages 721—731
DOI https://doi.org/10.2147/IDR.S195555
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Joachim Wink
Purpose: Cycloserine
has been used in multidrug-resistant tuberculosis (MDR-TB) treatment since the
1950s. We evaluated the efficacy and safety of cycloserine and sought to
clarify the role of cycloserine for treatment of simple MDR-TB, pre-extensively
drug-resistant tuberculosis (pre-XDR-TB), and extensively drug-resistant
tuberculosis (XDR-TB).
Materials and methods: A
retrospective observational study was performed in Zhejiang Province, China. We
enrolled 144 cycloserine-treated and 181 cycloserine-nontreated patients
consecutively and determined the treatment outcome as the primary outcome. The
proportion of patients with sputum culture conversion and the frequency of
adverse drug reactions were also assessed.
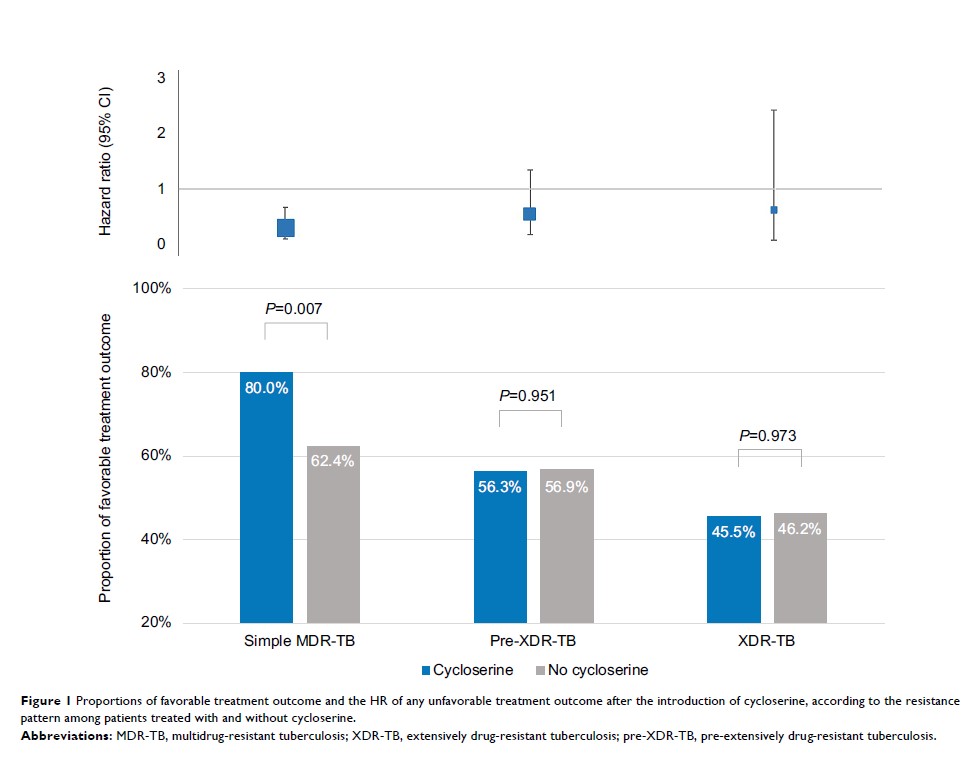
Results: One-hundred
(69.4%) out of 144 patients in the cycloserine group successfully completed
treatment. The HR of any unfavorable treatment outcome after the introduction
of cycloserine was 0.58 (95% CI: 0.38–0.86, P =0.008). Subgroup
analysis showed that cycloserine could benefit simple MDR-TB cases reducing the
risk of unfavorable treatment outcomes (HR: 0.43, 95% CI: 0.24–0.76, P =0.004), but not
pre-XDR-TB (HR: 0.65, 95% CI: 0.30–1.38, P =0.263) or XDR-TB
(HR: 0.73, 95% CI: 0.22–2.37, P =0.589). The culture conversion rate at the intensive
phase was similar whether cycloserine was administered or not (P =0.703). Of the
144 patients treated with cycloserine, a total of 16 (11.1%) patients
experienced side effects attributed to cycloserine.
Conclusion: Cycloserine
is an attractive agent for the treatment of MDR-TB, and its safety profile
warrants its use in most MDR-TB cases. Cycloserine significantly improved the
chance of a favorable outcome for patients with simple MDR-TB but not
pre-XDR-TB and XDR-TB. Thus, more aggressive regimens might be required for
pre-XDR-TB or XDR-TB patients.
Keywords: cycloserine,
multidrug-resistant tuberculosis, efficacy, safety, extensively drug-resistant
tuberculosis, treatment outcome