110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

基于炎症指标对于 FOLFOX 的化疗的结直肠癌患者的动态影响
Authors Tao Y, Yuan D, Pang H, Wu H, Liu D, Jin N, Wu N, Qiu J, Cao Y
Received 24 October 2018
Accepted for publication 20 February 2019
Published 10 April 2019 Volume 2019:11 Pages 2817—2829
DOI https://doi.org/10.2147/CMAR.S191712
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 2
Editor who approved publication: Professor Nakshatri
Background: Inflammatory
cellular response is implicated in the pathogenesis of colorectal cancer (CRC).
Nevertheless, the dynamic effects of inflammatory index coNLR
(neutrophil-to-lymphocyte ratio)-PLR (platelet-to-lymphocyte ratio) during
chemotherapy remain elusive.
Methods: The
baseline clinical data and laboratory parameters of 480 CRC patients who
received palliative resection of primary tumors and FOLFOX-based chemotherapy
from January 2007 to January 2013 were retrospectively analyzed. Receiver
operating characteristic curves were plotted to obtain the predictive NLR and
PLR values, and to calculate the coNLR-PLR score. The Kaplan–Meier method was
used to estimate the rates of recurrence-free survival (RFS) and overall
survival (OS), and the Cox proportional hazards model was employed for
analysis.
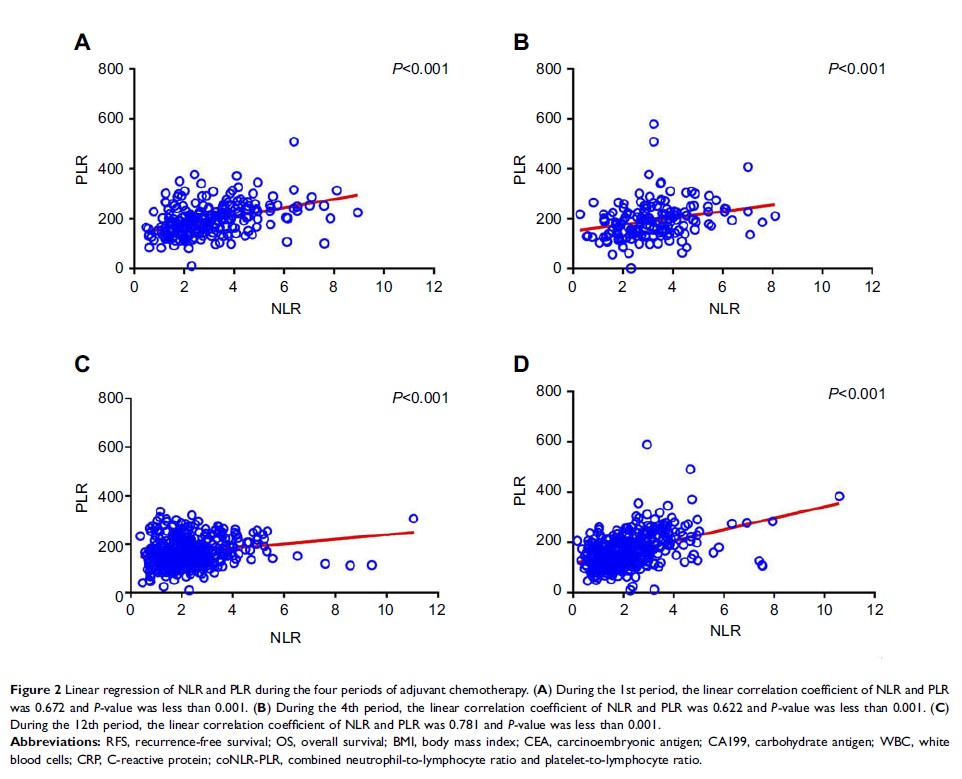
Results: The
dynamic cut-off values of NLR during four periods of chemotherapy were 3.029,
2.466, 2.102 and 1.795, respectively, and those of PLR were 216.438, 187.572,
169.027 and 174.368, respectively. A higher coNLR-PLR was significantly
associated with lower rates of RFS and OS (P <0.05). Both univariate and multivariate analyses
showed that coNLR-PLR was a significant independent prognostic factor for RFS
and OS (P <0.05).
Conclusions: CoNLR-PLR
was a significant prognostic predictor for CRC patients who received
FOLFOX-based chemotherapy. Evaluating this index can accurately predict the
clinical treatment outcomes after chemotherapy.
Keywords: colorectal
cancer, neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio,
FOLFOX-based chemotherapy, coNLR-PLR