110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

动脉瘤性蛛网膜下腔出血患者中性粒细胞与淋巴细胞比率与迟发性脑缺血的关系: 可能涉及脑血液灌注
Authors Wu Y, He Q, Wei Y, Zhu J, He Z, Zhang XD, Guo ZD, Xu R, Cheng C, Huang Z, Sun XC
Received 11 October 2018
Accepted for publication 14 February 2019
Published 26 April 2019 Volume 2019:15 Pages 1001—1007
DOI https://doi.org/10.2147/NDT.S190477
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Professor Jun Chen
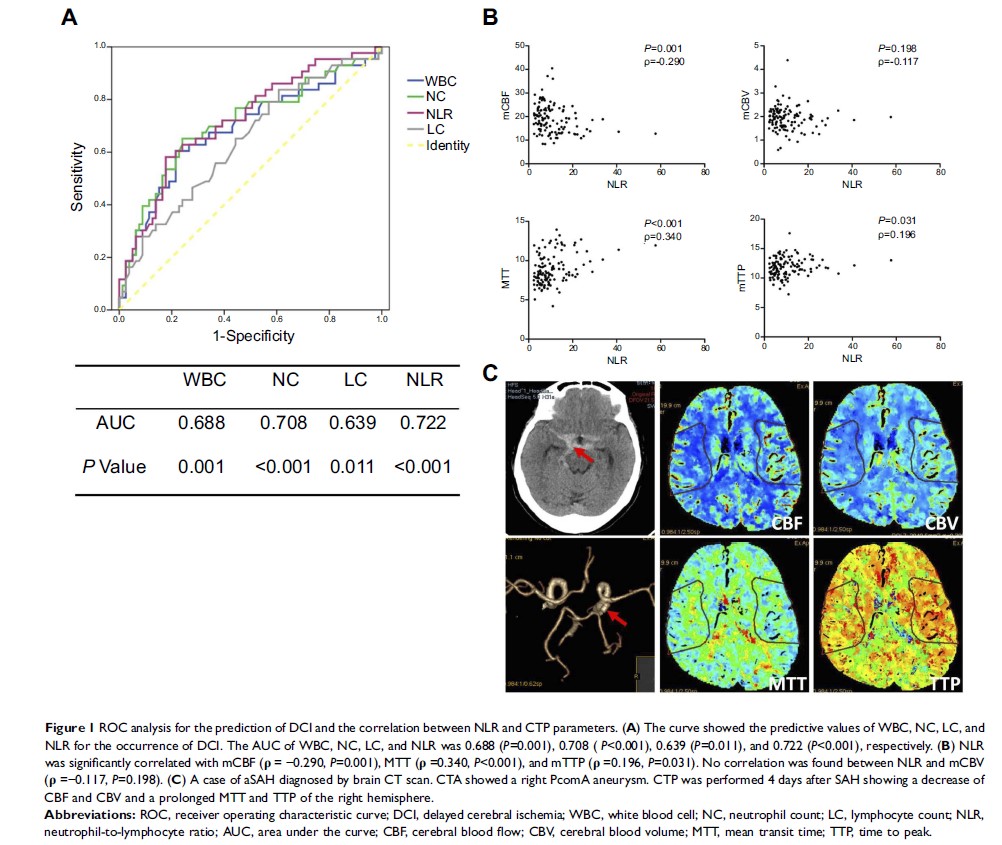
Background and purpose: Emerging
evidence suggests that systemic inflammation is associated with the
pathophysiological process of delayed cerebral ischemia (DCI) after aneurysmal
subarachnoid hemorrhage (aSAH). This study aimed to investigate the association
of white blood cell (WBC) count and neutrophil-to-lymphocyte ratio (NLR) with
the occurrence of DCI in SAH patients.
Methods: A total
of 122 patients diagnosed with aSAH within 72 h of onset were retrospectively
enrolled. The count of WBC, neutrophil count (NC), and lymphocyte (LC) was
collected on admission. Computed tomography perfusion was performed within 7
days after SAH. The occurrence of DCI was recorded during the hospitalization.
Results: Among
enrolled patients, 43 (35.2%) developed DCI during hospitalization. Patients
who developed DCI had a higher count of WBC, NC, and NLR as well as a lower
count of LC. NC and NLR were independently associated with the occurrence of
DCI, while NLR was the best predictive parameter according to the receiver
operating characteristic curve. Moreover, there was a strong correlation
between NLR and mean cerebral blood flow, mean transit time and mean time to
peak.
Conclusion: Leukocytosis
is an early pathology of SAH, and NLR may be a practical predictor for the
occurrence of DCI in SAH patients.
Keywords: aneurismal
subarachnoid hemorrhage, neutrophil-to-lymphocyte ratio, cerebral blood flow,
delayed cerebral ischemia