110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

The impact of increased post-progression survival on the cost-effectiveness of interventions in oncology
Authors Retzler J, Davies H, Jenks M, Kiff C, Taylor M
Received 18 October 2018
Accepted for publication 8 March 2019
Published 3 May 2019 Volume 2019:11 Pages 309—324
DOI https://doi.org/10.2147/CEOR.S191382
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Lorenzo Colombo
Purpose: Cost-effectiveness analyses (CEA) of new
technologies typically include “background” costs (eg, all “related” health
care costs other than the specific technology under evaluation) as well as drug
costs. In oncology, these are often expensive. The marginal cost-effectiveness
ratio (ie, the extra costs and QALYs associated with each extra period of
survival) calculates the ratio of background costs to QALYs during
post-progression. With high background costs, the incremental
cost-effectiveness ratio (ICER) can become less favorable as survival increases
and the ICER moves closer to the marginal cost-effectiveness ratio, making
cost-effectiveness prohibitive. This study assessed different methods to
determine whether high ICERs are caused by high drug costs, high “background
costs” or a combination of both and how different approaches can alter the
impact of background costs on the ICER where the marginal cost-effectiveness
ratio is close to, or above, the cost-effectiveness threshold.
Methods: The
National Institute for Health and Care Excellence oncology technology
appraisals published or updated between October 2012 and October 2017 were
reviewed. A case study was selected, and the CEA was replicated. Three modeling
approaches were tested on the case study model.
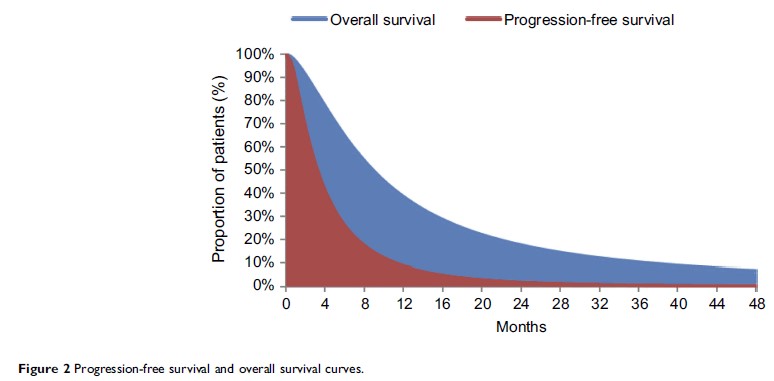
Results: Applying
one-off “transition” costs during post-progression reduced the ongoing
“incremental” costs of survival, which meant that the marginal
cost-effectiveness ratio was substantially reduced and problems associated with
additional survival were less likely to impact the ICER. Similarly, the use of
two methods of additional utility weighting for end-of-life cases meant that
the marginal cost-effectiveness ratio was reduced proportionally, again
lessening the impact of increased survival.
Conclusion: High
ICERs can be caused by factors other than the cost of the drug being assessed.
The economic models should be correct and valid, reflecting the true nature of
marginal survival. Further research is needed to assess how alternative
approaches to the measurement and application of background costs and benefits
may provide an accurate assessment of the incremental benefits of
life-extending oncology drugs. If marginal survival costs are incorrectly
calculated (ie, by summing total post-progressed costs and dividing by the
number of baseline months in that state), then the costs of marginal survival
are likely to be overstated in economic models.
Keywords: cancer,
cost, economics, overall survival, quality of life, modelling