110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

用于预测接受治愈性治疗的 II 期鼻咽癌患者总体生存率的诺模图开发和外部验证
Authors He SS, Wang CT, Peng ZW, Ren YF, Lu LX, Chen RW, Liang SB, Wang Y, Chen Y
Received 19 January 2019
Accepted for publication 29 March 2019
Published 10 May 2019 Volume 2019:11 Pages 4403—4412
DOI https://doi.org/10.2147/CMAR.S202151
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Melinda Thomas
Peer reviewer comments 3
Editor who approved publication: Dr Antonella D'Anneo
Objective: To
facilitate decision-making support for individual patients, development and
external validation of a nomogram was undertaken to reveal prognostic factors
and predict the value of concurrent chemoradiotherapy (CCRT) compared with
radiotherapy (RT) for stage-II nasopharyngeal carcinoma (NPC) patients.
Methods: Clinical
data of 419 and 309 patients with American Joint Committee on Cancer (2017)
stage-II NPC in two institutions in China were collected retrospectively.
Overall survival (OS) and progression-free survival were compared using
Kaplan–Meier estimates. Cox regression analysis was used to identify the
prognostic factors for building the nomogram. Predictive accuracy and
discriminative ability were measured using the Concordance Index.
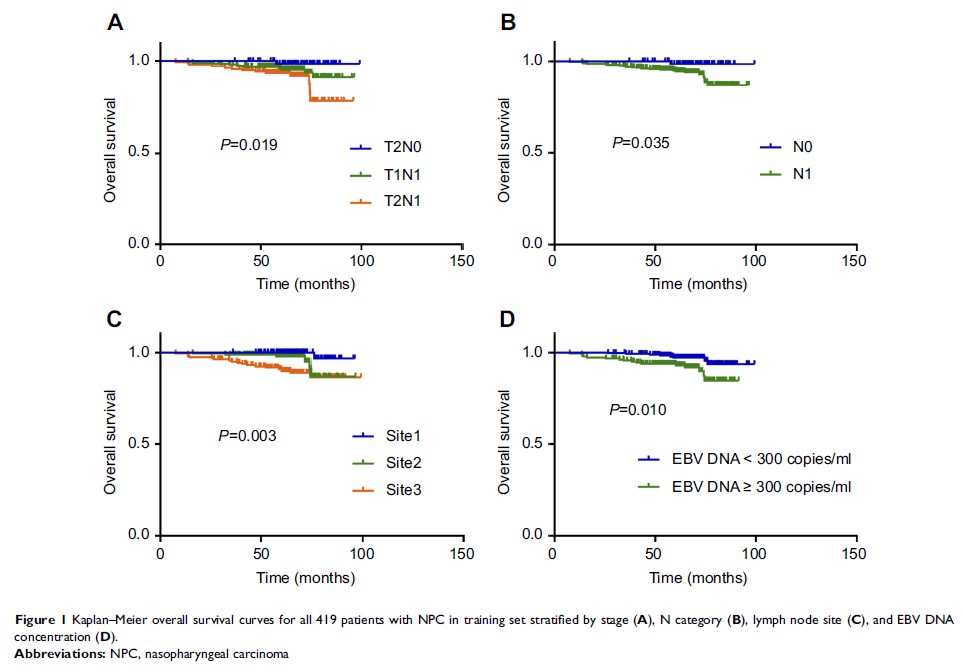
Results: Finally,
there were 24 and 20 deaths in the development and validation group,
respectively. Patients with stage T2N1, N1 stage, involvement of
retropharyngeal and unilateral cervical lymph nodes, and who had RT alone had
worse OS (P =0.019,
0.035, 0.003 and 0.010, respectively; log-rank test) than patients with stage
T1N1 and T2N0, N0 stage, involvement of retropharyngeal or unilateral cervical
lymph nodes, and CCRT, respectively. After multivariate analysis of the
training set, age, neutrophil-to-lymphocyte ratio, therapy type, and
pretreatment plasma concentration of Epstein–Barr virus DNA were independent
prognostic factors of OS. A nomogram was established externally by involving
all the factors stated above. The Concordance Index for the established nomogram
to predict the OS of the training set was 0.793 (95% CI 0.689–0.897), and 0.803
(95% CI 0.696–0.910) in the validation set.
Conclusion: These
data suggest that the nomogram was validated externally, could predict
long-term outcome accurately, and enable accurate stratification of risk groups
for stage-II NPC. Our model facilitated individualized care of NPC patients.
Keywords: chemotherapy,
nasopharyngeal carcinoma, nomogram, prognosis, radiotherapy