110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

外阴鳞癌神经浸润的预后意义
Authors Long Y, Yao DS, Wei YS, Wei CH, Chen XY
Received 23 December 2018
Accepted for publication 10 April 2019
Published 14 May 2019 Volume 2019:11 Pages 4461—4469
DOI https://doi.org/10.2147/CMAR.S198047
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Background: Perineural
invasion (PNI) is closely associated with poor survival in several types of
malignant tumours, but whether this is true in vulvar squamous cell carcinoma
(VSCC) is unclear. The aims of this study were to determine the prognostic
significance of PNI in patients with VSCC.
Patients and methods: We
retrospectively analysed clinico-pathological data on 105 patients with VSCC
(stages IB-IV) treated surgically at our medical center between 2005 and 2015.
Results: PNI was
detected in 30 (28.6%) patients, and it was significantly associated with
well-known clinical risk factors: large tumour size, depth of invasion,
lymphatic vascular space invasion (LVSI), and intra- or extra-nodal spread.
Significantly greater proportions of patients with PNI received adjuvant
therapy after surgery (P =0.001) or showed local recurrence (P =0.002).
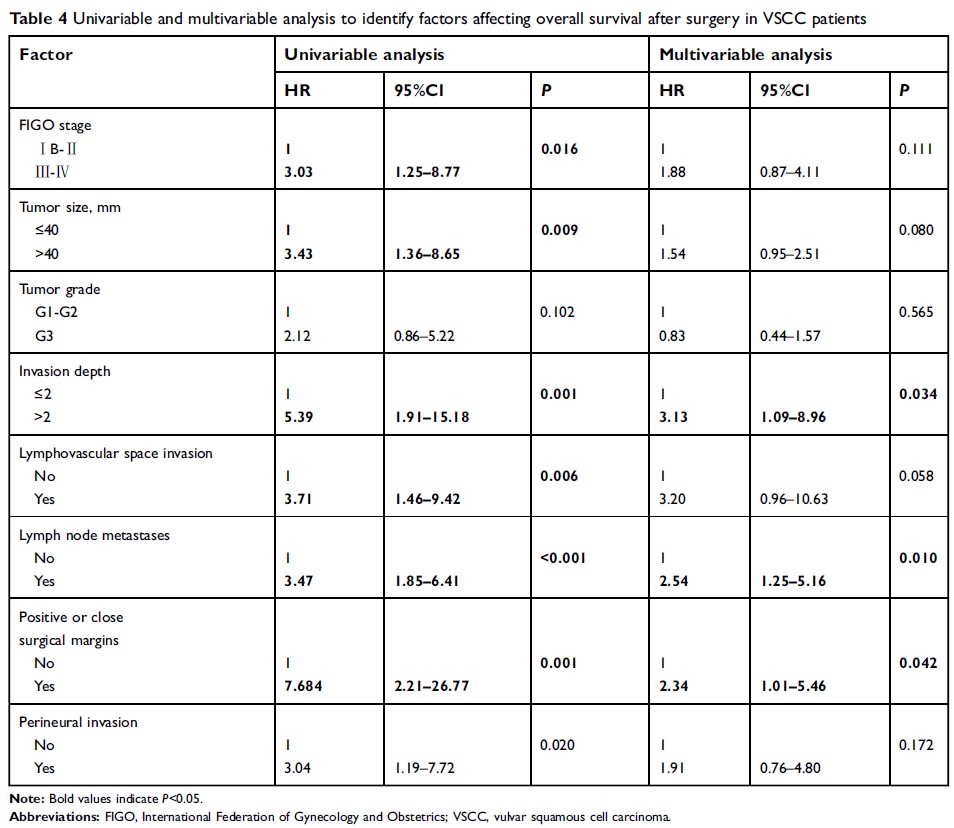
Multivariable analysis indicated that risk factors for disease-free survival
were tumour size (HR 3.02, 95%CI 1.75–7.75), LVSI (HR 4.82, 95%CI 1.36–17.07),
depth of invasion (HR 3.11, 95%CI 1.50–6.44), lymph node metastasis (HR 3.15,
95%CI 1.14–8.96) and positive or close surgical margins (HR 4.86, 95%CI
1.67–14.19). The latter three variables were also risk factors for overall
survival. PNI was associated with significantly shorter disease-free survival
(DFS) (P =0.020)
and overall survival (OS) (P =0.017) based on the log-rank test. Among patients
who received adjuvant treatment, Kaplan-Meier curves indicated no significant
differences between PNI-positive or -negative subgroups in disease-free
survival (P =0.085)
or overall survival (P =0.061). Based on multivariable analysis of all
patients, PNI was not a significant risk factor for either type of survival .
Conclusion: PNI in
VSCC is associated with significantly shorter disease-free and overall
survival, though it appears to be a weak independent predictor of worse
prognosis. Combining PNI with other risk factors may be useful for predicting
whether postoperative adjuvant therapy will be needed.
Keywords: Perineural
invasion, vulvar squamous cell carcinoma, adjuvant therapy, prognostic significance