110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

术前计算机断层扫描对 HBV 相关肝癌患者根治性切除术的预后价值
Authors Zhang W, Chen J, Liu L, Wang L, Liu J, Su D
Received 21 December 2018
Accepted for publication 5 March 2019
Published 16 May 2019 Volume 2019:12 Pages 3791—3804
DOI https://doi.org/10.2147/OTT.S199136
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Ms Rachel Predeepa
Peer reviewer comments 2
Editor who approved publication: Dr Federico Perche
Background: Preoperative
treatments are considered for patients with worse outcome to improve overall
survival and reduce tumor relapse. This study developed a prognostic risk
estimation for patients with hepatitis B virus (HBV)-related solitary
hepatocellular carcinoma after curative resection, including preoperative
computed tomography (CT) signatures.
Methods: Preoperative
multiphasic CTs for 166 patients with operable HCC were performed in our
hospital from 15 November 2013 through 15 May 2015. Follow-up information,
until 5 June 2017, included: CT, pathological and clinical characteristics, and
recurrence and metastases of HCC confirmed by pathological or radiological
diagnosis. The parameters were analyzed by the Kaplan-Meier method and Cox
proportional hazards regression analysis.
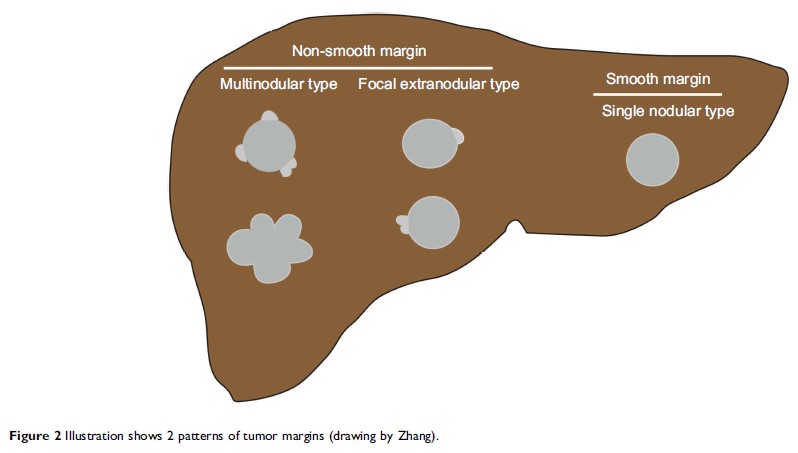
Results: In
multivariate analyses, overall survival was not significantly associated with
any of the analyzed prognostic risk factors, but did show that the following
were significant prognostic risk factors for disease-free survival: larger
tumor size, positive radiogenomic venous invasion, non-smooth tumor margin, and
histological microvascular invasion. These were all incorporated into the
nomogram. The calibration curves for predicting the probability of disease-free
survival between the nomogram and actual observation showed good conformity.
Conclusion: In
patients with HBV-related HCC, CT signatures were a noninvasive significant
indicator of disease-free survival. Thus, consideration of CT signatures may
optimize preoperative treatment strategies for the individual patient.
Keywords: hepatocellular
carcinoma, computed tomography, nomogram, prognosis