110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

谵妄的危险因素:治疗干预是其中的一部分吗?
Authors Xing J, Yuan Z, Jie Y, Liu Y, Wang M, Sun Y
Received 30 October 2018
Accepted for publication 8 April 2019
Published 17 May 2019 Volume 2019:15 Pages 1321—1327
DOI https://doi.org/10.2147/NDT.S192836
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 3
Editor who approved publication: Dr Yu-Ping Ning
Background: Delirium
is associated with increased morbidity and mortality in critically ill
patients. Research on risk factors for delirium allows clinicians to identify
high-risk patients, which is the basis for early prevention and diagnosis.
Besides the risk factors for delirium that are commonly studied, here we more
focused on the less-studied therapeutic interventions for critically ill
patients which are potentially modifiable.
Materials and methods: A total
of 320 non-comatose patients admitted to the ICU for more than 24 hrs during 9
months were eligible for the study. Delirium was screened once daily using the
CAM-ICU. Demographics, admission clinical data, and daily interventions were
collected.
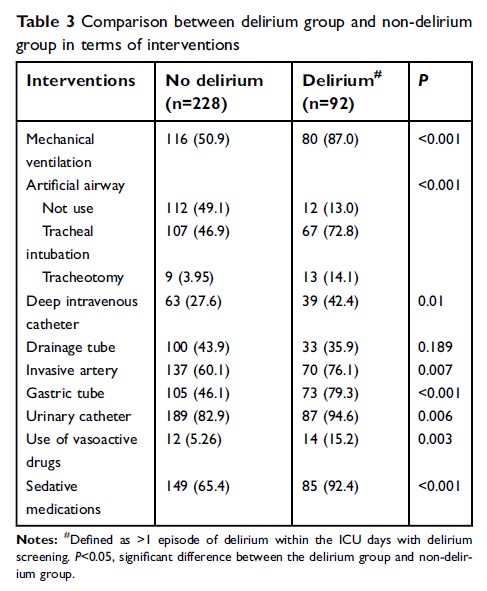
Results: Ninety-two
patients (28.75%) experienced delirium at least once. Delirious patients were
more likely to have longer duration of mechanical ventilation, ICU stay, and
hospital stay. Most of the less-studied therapeutic interventions were linked
to delirium in the univariate analysis, including gastric tube, artificial
airway, deep intravenous catheter, arterial line, urinary catheter, use of
vasoactive drugs, and sedative medication. After adjusting with age and ICU
length of stay, mechanical ventilation (OR: 5.123; 95% CI: 2.501–10.494), Acute
Physiology and Chronic Health Evaluation (APACHE) II score≥20 at admission (OR:
1.897; 95% CI: 1.045–3.441), and gastric tube (OR: 1.935, 95% CI: 1.012–3.698)
were associated with increased risk of delirium in multivariate analysis.
Conclusion: Delirium
was associated with prolonged mechanical ventilation, ICU stay, and hospital
stay. Multivariate risk factors were gastric tube, mechanical ventilation, and
APACHE II score. Although being a preliminary study, this study suggests the
necessity of earliest removal of tubes and catheters when no longer needed.
Keywords: delirium,
critical care, intensive care unit, risk factors, prevention