110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

中国老年人接受胸腹部大手术后的虚弱和术后并发症
Authors Han B, Li Q, Chen X
Received 10 January 2019
Accepted for publication 25 March 2019
Published 22 May 2019 Volume 2019:14 Pages 947—957
DOI https://doi.org/10.2147/CIA.S201062
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Amy Norman
Peer reviewer comments 3
Editor who approved publication: Dr Zhi-Ying Wu
Purpose: To
determine the association between frailty and postoperative complications in
elderly Chinese patients and to determine whether addition of frailty
assessment improves the predictive ability of the American Society of
Anesthesiologists (ASA) score, Physiological and Operative Severity Score for
the Enumeration of Mortality and Morbidity (POSSUM), and Estimation of
Physiologic Ability and Surgical Stress (E-PASS) score.
Patients and methods: A
prospective cohort study was conducted in a tertiary hospital. Elderly patients
undergoing major thoracic or abdominal surgery were included. Frailty phenotype
and ASA, POSSUM, and E-PASS scores were assessed. Demographic, preoperative,
and surgical variables were extracted from medical records. Primary outcome
measure was in-hospital Clavien-Dindo ≥ grade II complications. Multiple
logistic regression was used to examine the association between frailty and
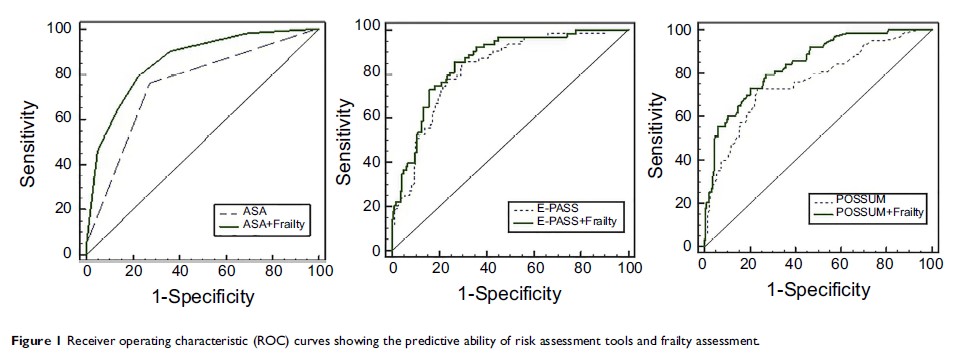
complications. Receiver operating characteristic curves were used to explore
the predictive ability of frailty.
Results: Prevalence
of frailty was 26.12%. Significant differences were observed between the frail
and non-frail groups with respect to age, Activities of Daily Living, Charlson
Comorbidity Index, respiratory function, presence of malignancy, serum albumin,
prealbumin, and hemoglobin levels (P <0.05). ASA, POSSUM, and E-PASS scores were higher
in the frail group. After adjusting for all covariates, frailty was
significantly associated with postoperative complications in hospital [odds
ratio: 16.59, 95% CI: 4.56–60.40, P <0.001]. The area under the curve (AUC) for
frailty was 0.762 (95% CI: 0.703–0.814). The AUC for ASA, POSSUM, and E-PASS
for prediction of complications was 0.751 (95% CI: 0.692–0.804), 0.762 (95% CI:
0.704–0.814), and 0.824 (95% CI: 0.771–0.870), respectively. Addition of
frailty assessment increased the AUC to 0.858 (95% CI: 0.808–0.899), 0.842 (95%
CI: 0.790–0.885), and 0.854 (95% CI: 0.803–0.896), respectively.
Conclusion: Frailty
is an effective predictor of postoperative complications in elderly Chinese
patients undergoing major thoracic and abdominal surgery. Frailty assessment
can improve the predictive ability of current surgical risk assessment tools.
Frailty phenotype should be considered perioperatively. Frailty assessment
could also expand the scope for nurses to evaluate patients for safety
management.
Keywords: frailty
assessment, risk assessment tool, surgery, postoperative complication