110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

中国 ALK/EGFR 突变肺癌患者治疗频率、临床特征和鉴别反应
Authors Liu J, Mu Z, Liu L, Li K, Jiang R, Chen P, Zhou Q, Jin M, Ma Y, Xie Y, Xiang J, Li B, Ma Y, Mao X, Zhang L, Zhang T, Wu D
Received 27 November 2018
Accepted for publication 7 April 2019
Published 23 May 2019 Volume 2019:13 Pages 1809—1817
DOI https://doi.org/10.2147/DDDT.S196189
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Cristiana Tanase
Purpose: EGFR and anaplastic lymphoma
kinase (ALK ) alterations have been
regarded as oncogenic drivers and incorporated into clinical practices to
manage nonsmall cell lung cancer (NSCLC). Alterations of these two genes were
traditionally considered to be mutually exclusive, but recent studies have
suggested that they can occur concomitantly. Here, we investigated the
prevalence, clinical features and outcomes in response to the treatment of
NSCLC patients who harbor EGFR and ALK co-alterations.
Methods: We reviewed the genomic profiles of 419 ALK -rearranged NSCLC patients with
the intent of investigating the EGFR kinase
domain (exon 18–21) and ALK co-alterations.
The genomes of these patients were sequenced in a Clinical Laboratory
Improvement Amendments-certified laboratory.
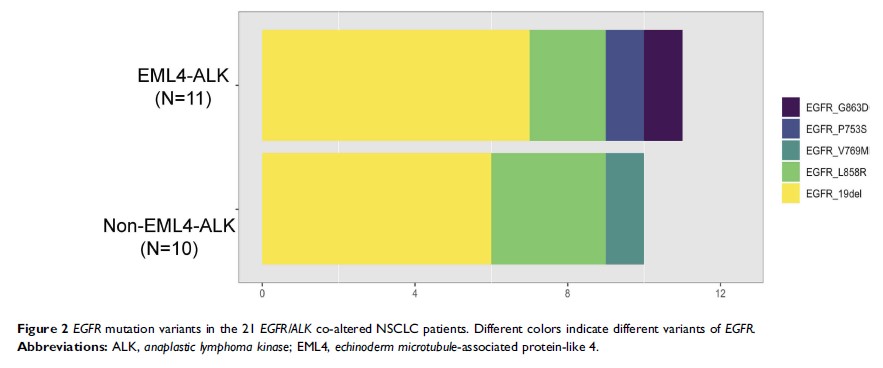
Results: The overall frequency of concomitant EGFR (exon 18–21) and ALK alterations was 5.01%
(21/419) in ALK -rearranged
NSCLC patients. The concomitant rate of EGFR alterations
in patients with EML4-ALK co-alterations
(3.06%, 11/359) was dramatically lower than that in patients with non-EML4-ALK co-alterations
(16.67%, 10/60, p <0.01). EML4-ALK/EGF R co-alterations were
more prone to occur in females than in males, and non-EML4-ALK/EGFR co-alterations were more
common in males than in females (p =0.02). Before the
detection of EGFR-ALK co-alterations,
some patients were treated with EGFR-TKIs (n=16) according to previously
detected EGFR alterations;
Kaplan–Meier analysis revealed that EML4-ALK/EGFR co-altered patients
(n=7) had a significantly shorter progression-free survival (PFS) after
EGFR-TKI treatment than that of non-EML4-ALK/EGFR co-altered patients
(n=8; mPFS, 6.0 vs 15.0 months, p =0.046). In
addition, we demonstrated the subsequent clinical outcomes of co-altered
patients after previous EGFR-TKI treatment. Five EGFR/ALK co-altered
patients treated with single TKIs (EGFR-TKIs or ALK-TKIs) displayed diverse
clinical outcomes. Three patients who received dual-TKI treatment (EGFR-TKI
plus ALK-TKI) all achieved a PFS of more than 5 months (8.4 months, 8.6 months,
>5.2 months).
Conclusion: EML4-ALK/EGFR and
non-EML4-ALK/EGFR co-alterations
displayed distinct clinical features and responses to EGFR-TKIs, suggesting
that non-EML4-ALK co-alterations are
likely to occur as a resistance mechanism to EGFR-TKI. In addition, dual-TKI
therapy might be a better choice than single-TKI treatments for these
co-altered patients. To the best of our knowledge, this is the largest
dual-positive EGFR/ALK cohort
study in People’s Republic of China.
Keywords: EGFR alteration, ALK rearrangement, nonsmall
cell lung cancer, EML4-ALK, tyrosine kinase inhibitor