110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

特立帕肽对中国和白种人骨质疏松症患者的影响:疗效的桥接研究
Authors Xie Z, Chen Y, Gurbuz S, Zhang B, Li Y, Bai F, Chen Y
Received 8 August 2018
Accepted for publication 1 November 2018
Published 27 May 2019 Volume 2019:14 Pages 959—968
DOI https://doi.org/10.2147/CIA.S181929
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Objective: To bridge
the efficacy and compare the safety of the 24-week teriparatide treatment in a
Chinese osteoporosis study (NCT00414973) to a large international trial (FPT,
NCT00670501) to determine whether long-term results from the international
study were applicable to Chinese patients.
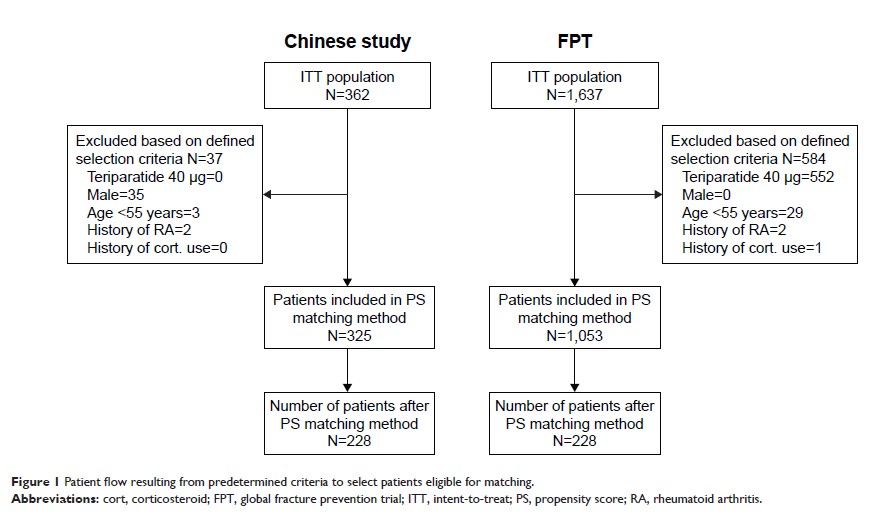
Methods: In this
post-hoc analysis, a propensity score matching method was used to select
patients with similar baseline characteristics. Patients were female with
osteoporosis at high risk of fracture, aged ≥55 years, and had no history
of rheumatoid arthritis or corticosteroid use. Outcomes included percentage
changes in lumbar-spine bone mineral density (LS-BMD) from baseline to
24 weeks, safety in matched-pair patients, and long-term percentage
changes in LS-BMD and fragility fracture incidence in the matched fracture
prevention trial (FPT) population. The determination of the acceptability of
bridging results was based on the International Conference on Harmonization E5
guidelines.
Results: A total
number of 228 patients from each study were matched and paired. Patients were
similar at baseline (P -values >0.33) except for ethnicity (98% Caucasian
for FPT). For changes in LS-BMD from baseline to week 24, treatment with
teriparatide showed significantly greater increases (P -values <0.001;
least-squares mean difference: 5.0% in the Chinese study and 5.4% in FPT) than
comparator (calcitonin/placebo). The safety profiles over 24 weeks were
similar between two studies. For matched-pair FPT patients, long-term changes
in LS-BMD were significantly greater (least-squares mean difference:
11.5%, P <0.001)
and the fragility fracture rate was marginally lower in the teriparatide group
compared with the placebo group (13.1% vs 22.3%, P =0.070).
Conclusion: Assuming
similar pharmacokinetic profiles for teriparatide between populations,
comparable increases in LS-BMD and consistent safety profiles within
24 weeks of the treatment suggest long-term LS-BMD results from the FPT
may be applicable to Chinese population.
Keywords: osteoporosis,
teriparatide, bridging, lumbar spine-bone mineral density, LS-BMD, fracture
prevention trial