110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

并发的 TP53 突变预测中国晚期 NSCLC 患者 EGFR-TKI 预后不良
Authors Hou H, Qin K, Liang Y, Zhang C, Liu D, Jiang H, Liu K, Zhu J, Lv H, Li T, Zhang X
Received 14 January 2019
Accepted for publication 30 April 2019
Published 21 June 2019 Volume 2019:11 Pages 5665—5675
DOI https://doi.org/10.2147/CMAR.S201513
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Cristina Weinberg
Peer reviewer comments 4
Editor who approved publication: Professor Nakshatri
Purpose: The study investigated the impact of TP53 mutations on the clinical efficacy of first-generation EGFR-tyrosine kinase inhibitors (TKIs) in Chinese patients with advanced or recurrent non-small-cell lung cancer (NSCLC).
Patients and methods: Tissues from 163 NSCLC patients at the Affiliated Hospital of Qingdao University were analyzed by next-generation sequencing (NGS) to determine the mutational status of EGFR and concurrent genetic alterations. TP53 mutations were evaluated in relation to baseline patient characteristics and treatment outcomes (progression-free survival [PFS], overall survival [OS], objective response rate [ORR] and disease control rate [DCR]).
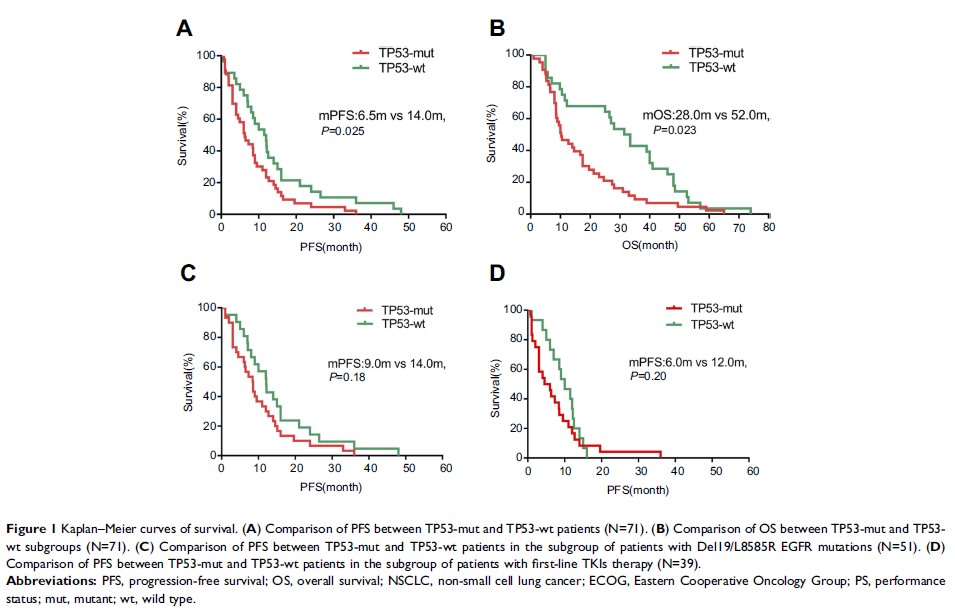
Results: Among 163 patients with advanced NSCLC, 77 were identified as EGFR-mutant (47.2%). Six patients who did not receive TKI treatment were excluded. Among the remaining 71 patients with EGFR genetic alterations, the frequency of pathogenic TP53 mutations was 60.6% (43/71), while other concurrent mutations were rare events. Markedly shorter median PFS (mPFS) (6.5 versus 14.0 months, P =0.025) and median OS (mOS) (28.0 versus 52.0 months, P =0.023) were observed in TP53-mut patients than in TP53-wt controls. The overall DCR and ORR of TP53-mutant patients were both lower than those of the TP53-wt cases (DCR: 76.7% versus 89.3%, P =0.160; ORR: 25% versus 28%, P =0.374). Differences in prognosis were significant, especially in the subgroup of patients with TP53 non-missense mutations, non-disruptive mutations, mutations in exon 6, mutations in exon 7 and mutations in the non-DBD region among all TP53 mutations.
Conclusion: TP53 mutations reduce responsiveness to TKIs and worsen the prognosis of EGFR-mutant NSCLC patients, especially for those with non-missense mutations and non-disruptive mutations, as well as mutations in exon 6, exon 7 and non-DBD region, thus acting as an independent predictor of poor outcome in advanced NSCLC patients treated with first-generation TKI therapy. Our study also suggests that TP53 mutation might be involved in primary resistance to EGFR-TKIs in Chinese NSCLC patients.
Keywords: TP53, epidermal growth factor receptor, tyrosine kinase inhibitors, non-small-cell lung cancer, mutation, exon