111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

使用奥希替尼及其后续耐药机制成功治疗 AC0010 诱导的间质性肺病恢复后的非小细胞肺癌患者获得性 EGFR T790M 突变
Authors Wang H, Zhang L, Shi X, Zhang X, Si X
Received 9 February 2019
Accepted for publication 17 June 2019
Published 10 July 2019 Volume 2019:12 Pages 5545—5549
DOI https://doi.org/10.2147/OTT.S204689
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Jyoti Bajaj
Peer reviewer comments 2
Editor who approved publication: Dr Arseniy Yuzhalin
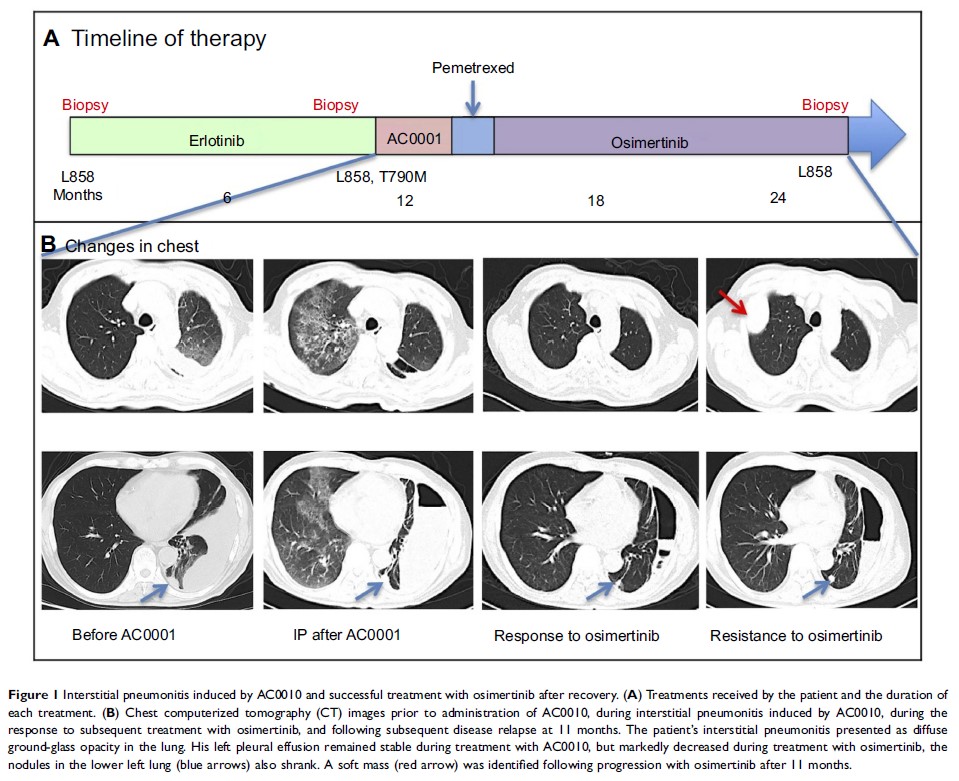
Objective: Treatment with epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKIs)can occasionally lead to interstitial lung disease (ILD), and the appropriate treatment after recovery from ILD remains controversial. AC0010 is an investigational third-generation TKI used in China to selectively target the T790M mutation. Here, we describe a patient who developed ILD after AC0010 treatment and was then successfully re-challenged with osimertinib.
Methods: The patient was a 67-year-old male with a diagnosis of metastatic pulmonary adenocarcinoma with an L858R mutation on exon 21. Acquired T790M mutation was confirmed by re-biopsy after progression on erlotinib treatment. The patient was treated with AC0010, and developed ILD 54 days after treatment initiation. Following his recovery from ILD, osimertinib (80 mg/day) was administered with no adverse effects. After progression on osimertini11 months later, a histological transformation from adenocarcinoma to large-cell neuroendocrine carcinoma was confirmed by re-biopsy, with a marked increase in serum neuron-specific enolase.
Conclusions: This is the first report of interstitial pneumonitis caused by AC0010. Osimertinib re-challenge after recovery from ILD was a safe and effective treatment option. Our report further highlights that pathological transformation of large-cell neuroendocrine carcinoma represents one of the resistance mechanisms of osimertinib, and may be accompanied by an increase in serum neuron-specific enolase.
Keywords: osimertinib, AC0010, interstitial lung disease, resistance mechanism, transformation, large-cell neuroendocrine carcinoma