110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

阿司匹林作为心血管疾病的一级预防剂的功效和安全性:最新的荟萃分析
Authors Xie W, Luo Y, Liang X, Lin Z, Wang Z, Liu M
Received 16 December 2018
Accepted for publication 20 August 2019
Published 24 September 2019 Volume 2019:15 Pages 1129—1140
DOI https://doi.org/10.2147/TCRM.S198403
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Ms Justinn Cochran
Peer reviewer comments 2
Editor who approved publication: Professor Deyun Wang
Purpose: Information regarding the use of aspirin for patients with no known cardiovascular disease remains conflicting. We performed an updated meta-analysis to evaluate the efficacy and safety of aspirin for primary prevention of cardiovascular disease.
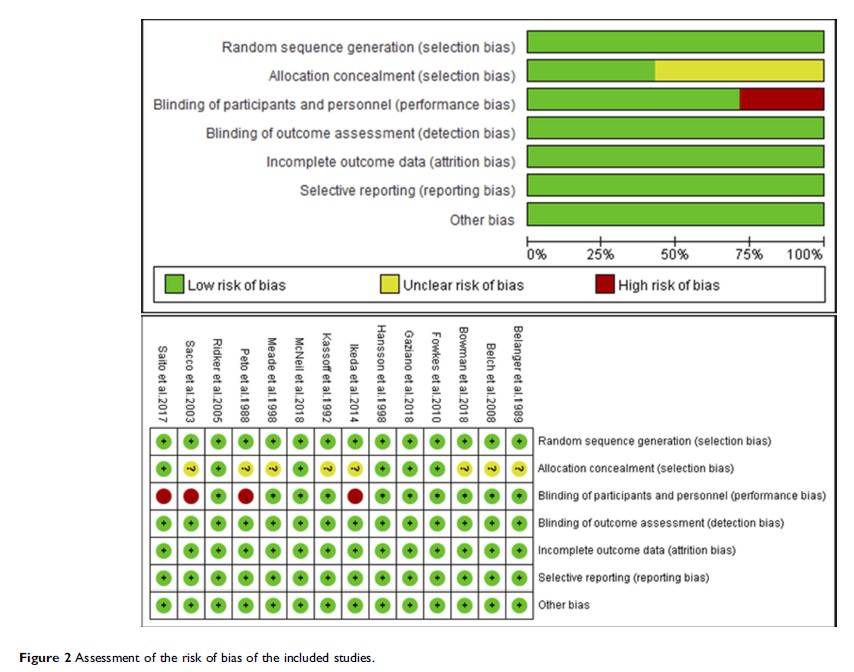
Patients and methods: PubMed, MEDLINE, and Cochrane library databases were searched for randomized controlled trials comparing aspirin with placebos or no treatment published up until November 1, 2018. The primary efficacy endpoint was all-cause death. The secondary endpoints included cardiovascular death, myocardial infarction, and stroke. The safety endpoints included major bleeding, gastrointestinal bleeding, and hemorrhagic stroke.
Results: Fourteen studies were included. Aspirin use was associated with a lower risk of myocardial infarction than placebo use or no treatment (risk ratio [RR], 0.83, 95% confidence interval [CI]: 0.73–0.95, P = 0.005). Additionally, compared with the control groups, aspirin use was not associated with a lower risk of all-cause mortality or cardiovascular mortality. In terms of safety, aspirin use was associated with a higher risk of major bleeding (RR, 1.40, 95% CI: 1.25–1.57, P = 0.000), gastrointestinal bleeding (RR, 1.58, 95% CI: 1.25–1.99, P = 0.000), and hemorrhagic stroke (RR, 1.30, 95% CI: 1.06–1.60, P = 0.011). Furthermore, the treatment effect was not significantly modified by patients’ clinical characteristics. No publication bias was present.
Conclusion: Aspirin use reduced the myocardial infarction risk in patients without known cardiovascular disease, but had no effect in terms of reducing the risk of all-cause death, cardiovascular death, and stroke, and increased the risk of major bleeding, gastrointestinal bleeding, and hemorrhagic stroke.
Keywords: aspirin, primary prevention, cardiovascular disease, meta-analysis