111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

小体积前列腺癌和膀胱出口梗阻患者术后下尿路症状改善的预测指标
Authors Li XD, Wu YP, Ke ZB, Lin TT, Chen SH, Xue XY, Xu N, Wei Y
Received 13 June 2019
Accepted for publication 15 October 2019
Published 7 November 2019 Volume 2019:15 Pages 1291—1304
DOI https://doi.org/10.2147/TCRM.S219331
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Nicola Ludin
Peer reviewer comments 2
Editor who approved publication: Professor Deyun Wang
Objective: To explore the factors associated with improvement of lower urinary tract symptoms (LUTS) after transurethral plasmakinetic enucleation of the prostate (PKEP) and transurethral resection of the prostate (TURP) in patients with a small-volume prostate and bladder outlet obstruction (BOO).
Methods: The clinicopathologic data of 257 patients with BOO and a small-volume prostate from January 2013 to January 2018 were retrospectively collected preoperatively, 3 months postoperatively, and 12 months postoperatively. Patients were divided into postoperative success and failure groups based on the IPSS, IPSS-v, and IPSS-s. The relationship between each parameter and the improvement of postoperative LUTS was analyzed. Subgroup analysis was performed to compare the differences between the TURP and PKEP groups.
Results: Among patients followed up for 3 months postoperatively, multivariate analysis demonstrated that IPP, PUA, and post-PCB were significant predictors of postoperative IPSS improvement; TZI, IPP, and PUA were significant predictors of postoperative IPSS-v improvement; post-PCB and the surgical procedure were significant predictors of IPSS-s improvement; and IPP and PUA were significant predictors of postoperative Qmax improvement. Among patients followed up for 12 months postoperatively, multivariate analysis revealed that IPP, PUA, and post-PCB were significant predictors of postoperative IPSS improvement; PUA was a significant predictor of postoperative IPSS-v improvement; post-PCB was a significant predictor of IPSS-s improvement; and IPP and PUA were significant predictors of postoperative Qmax improvement. The post-PCB was significantly lower in the PKEP than the TURP group and the prostatic calculi removal rate was significantly higher in the PKEP than the TURP group.
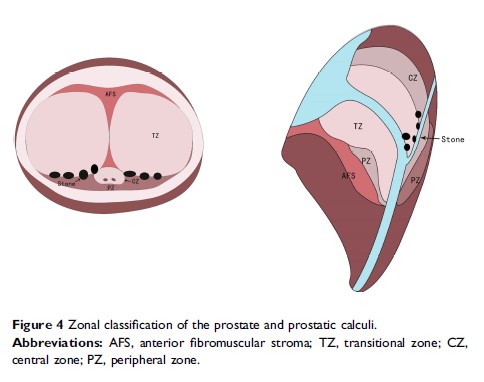
Conclusion: Patients with a greater preoperative IPP and PUA and smaller post-PCB showed greater improvement of postoperative LUTS. PKEP might help to remove calculi from between the transitional and peripheral zones of prostate. Compared with conventional TURP, PKEP may improve the early postoperative storage symptoms of LUTS in patients with a small-volume prostate and BOO.
Keywords: small-volume prostate, lower urinary tract symptoms, International Prostate Symptom Score