111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

原发性中枢神经系统肿瘤的神经转移:单中心 198 例临床病理和放射学特征回顾
Authors Liu H, Zhang J, Liu Y, Sun Y, Li C, Gu C, Wang H, Zhang H, Yu C, Zhang M
Received 29 May 2019
Accepted for publication 26 October 2019
Published 20 November 2019 Volume 2019:11 Pages 9829—9841
DOI https://doi.org/10.2147/CMAR.S217672
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Colin Mak
Peer reviewer comments 3
Editor who approved publication: Dr Eileen O'Reilly
Background: Neuraxis metastases (NM) from systemic and central nervous system (CNS) tumors have become increasingly common. However, a lack of systematic information restricts the development of the accurate diagnosis and treatment. The aim of this study is to facilitate the understanding of NM arising from CNS tumors in the largest cohort.
Methods: Based on the clinicopathological and neuroimaging findings, we retrospectively analyze the epidemiological characters, radiographic classification, therapeutic strategies and prognostic factors.
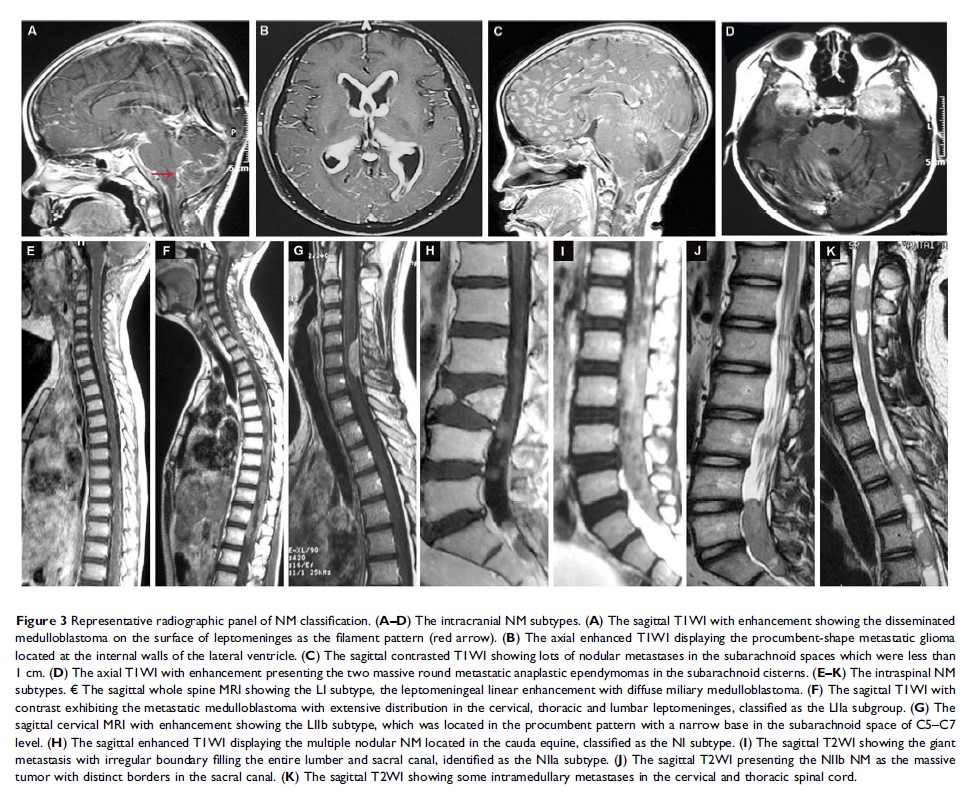
Results: A total of 198 cases are enrolled and the most common primary tumor is medulloblastoma (34.34%). The median age is 15.0 years and the majority of NM (79.29%) occur in the children and young adult groups. One hundred and forty-nine (75.25%) cases suffer from intracranial metastases, and 169 (85.35%) have intraspinal NM. The whole leptomeninges and cauda equine are the most preferential disseminated sites. Upon MRI parameters, the massive and miliary subgroup occurs most frequently in the intracranial and intraspinal NM, respectively. Treatment includes surgery (21.71%), chemotherapy alone (19.19%), radiation alone (10.10%) and combined therapy (55.56%). Operations are performed in order to identify pathology and relive masses, as well as the triple chemotherapeutic scheme consisting of ifosfamide, carboplatin and etoposide is recommended for most of NM. The median overall survival is 11.6 months. Younger age, coexistence of NM with primary tumors, shorter interval from primaries to metastases, glioma, leptomeningeal seeding and nodal subtype on MRI significantly correlate with poor prognosis.
Conclusion: In spite of controversial therapies and poor outcomes, the neuroimaging classification and comprehensive treatment contribute to the efficient administration of NM.
Keywords: neuraxis metastases, survival, MRI, classification, operation