111314
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

胸腔恶性肿瘤放疗期间使用血清标志物进行放射性肺炎风险的临床管理
Authors Deng Y, Qiu T, Patel N, Zhou S, Xue T, Zhang H
Received 21 September 2019
Accepted for publication 26 November 2019
Published 5 December 2019 Volume 2019:11 Pages 10249—10256
DOI https://doi.org/10.2147/CMAR.S231995
Checked for plagiarism Yes
Review by Single-blind
Peer reviewers approved by Dr Shashank Kaushik (PT)
Peer reviewer comments 2
Editor who approved publication: Professor Rudolph Navari
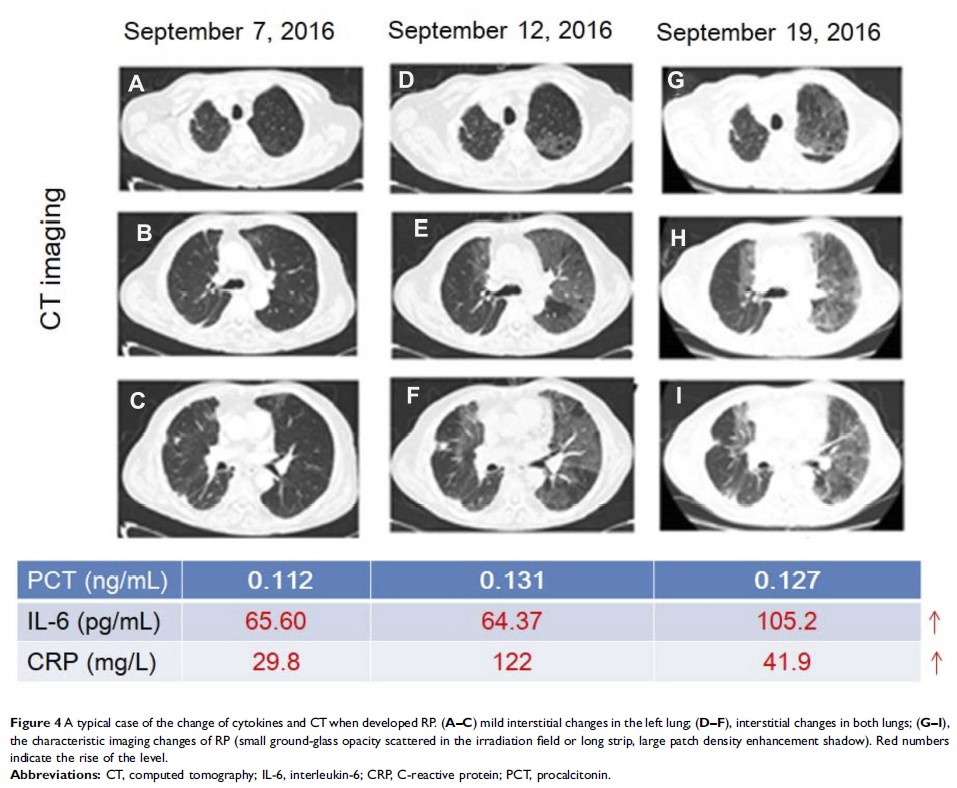
Purpose: Risk of radiation pneumonia (RP) could not be effectively detected due to non-specific clinical symptoms in the early stage. The purpose of this investigation was to evaluate serum biomarkers of cytokines interleukin-6 (IL-6), C-reactive protein (CRP) and procalcitonin (PCT) for its early detection in patients with thoracic malignant tumors receiving radiotherapy.
Patients and methods: The clinical data of 105 patients with thoracic malignant tumors (lung cancer, esophageal carcinoma and mediastinal tumors) treated by radiotherapy were retrospectively analyzed. The patients were divided into RP group and non-RP group according to the Common Terminology Criteria for Adverse Events (CTCAE 5.0). The serum level of IL-6 was detected by chemiluminescence, and the level of CRP was measured by nephelometry during radiotherapy. The level of PCT, one of the specific indicators to distinguish infection and non-infectious etiologies, was also detected by chemiluminescence.
Results: Among 105 patients treated by radiotherapy, 28 developed RP, and the other 77 had no RP. There was no significant difference in the risk of RP between patients’ factors (age, sex, PS score, smoking, tumor type) and treatment factors (chemotherapy, V5, GTV dose). However, chronic obstructive pulmonary disease (COPD), V20 and mean lung dose (MLD) were significantly different between the two groups (χ 2 = 4.131, 3.986, 7.830, P < 0.05). Furthermore, PCT levels were also found to have insignificant differences between RP group and non-RP group (P > 0.05). However, there were significant differences between the groups in the levels of IL-6 and CRP (P < 0.05). The IL-6 levels significantly increased earlier than that of conventional CT imaging when patients suffering from RP and peaked at 6 weeks during radiotherapy. CRP had a similar change as IL-6. Single cytokine and combination of IL-6 and CRP possessed a good ability to predict RP with the AUC of IL-6 of 0.89±0.04 (95% CI, 0.80–0.95, P<0.001), CRP of 0.87±0.05 (95% CI, 0.78–0.94, P<0.001), IL-6 + CRP of 0.92 ± 0.03 (95% CI, 0.83–0.97, P < 0.001), respectively.
Conclusion: The combined detection of serum IL-6, CRP and PCT may be an effectual method for early detection and clinical practice management of risk of RP.
Keywords: cancer, radiotherapy, radiation pneumonitis, interleukin-6, C-reactive protein, procalcitonin, biomarkers