110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

心脏移植受者中免疫抑制剂不依从性的患病率和危险因素:一个单中心横断面研究
Authors Zhang M, Zhou H, Nelson RS, Han Y, Wang Y, Xiang H, Cai J, Zhang J, Yuan Y
Received 19 July 2019
Accepted for publication 9 December 2019
Published 20 December 2019 Volume 2019:13 Pages 2185—2193
DOI https://doi.org/10.2147/PPA.S223837
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Background: Immunosuppressant nonadherence (INA) has been shown to affect outcomes after solid organ transplantation. The aim of the present study was to determine the prevalence of INA in heart transplant recipients and the associated risk factors of INA.
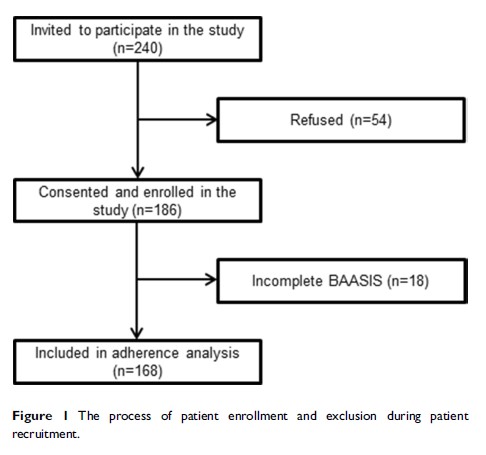
Methods: Adult heart transplant recipients who firstly received heart transplantation (discharged for at least 3 months) were consecutively enrolled. Immunosuppressant adherence was assessed using the Basel Assessment of Adherence with Immunosuppressive Medication Scale (BAASIS). INA was categorized into five domains of contributing factors (socio-demographic factors, transplant-related factors, healthcare system access factors, post-transplant treatment-related factors, and patient-related psychosocial factors). These factors were compared between adherent and nonadherent patients. The risk factors of INA were investigated by logistic regression analysis.
Results: A total of 168 heart recipients were ultimately included. Among them, 69 (41.1%) recipients were revealed to be nonadherent. Logistic regression analysis indicated that INA was associated with monthly income<3000 Chinese Yuan (CNY) (OR, 3.11; 95% CI, 1.58–6.12; p=0.001), number of prescribed concomitant drugs (OR, 1.23; 95% CI, 1.12–1.50; p=0.003) and concerns about immunosuppressants (OR, 1.09; 95% CI, 1.01–1.18; p=0.031).
Conclusions: Heart recipients had a high prevalence of INA. Lower income, greater number of prescribed concomitant drugs, and more concerns about immunosuppressants correlated most with timing nonadherence and taking nonadherence among heart recipients. These findings will be helpful to intervene on and prevent future INA of heart recipients.
Keywords: heart transplantation, immunosuppressants, adherence, risk factors, interventions