110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

外周血嗜酸性粒细胞作为慢性阻塞性肺疾病急性加重患者预后的生物标志物
Authors Wu HX, Zhuo KQ, Cheng DY
Received 11 August 2019
Accepted for publication 10 December 2019
Published 24 December 2019 Volume 2019:14 Pages 3003—3015
DOI https://doi.org/10.2147/COPD.S226783
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Chunxue Bai
Purpose: Mounting evidence suggests that eosinophil levels correlate with the effects of therapy and phenotype for chronic obstructive pulmonary disease (COPD). This study aimed to clarify the relationship between eosinophil levels and clinical outcomes in patients with acute exacerbation of COPD (AECOPD).
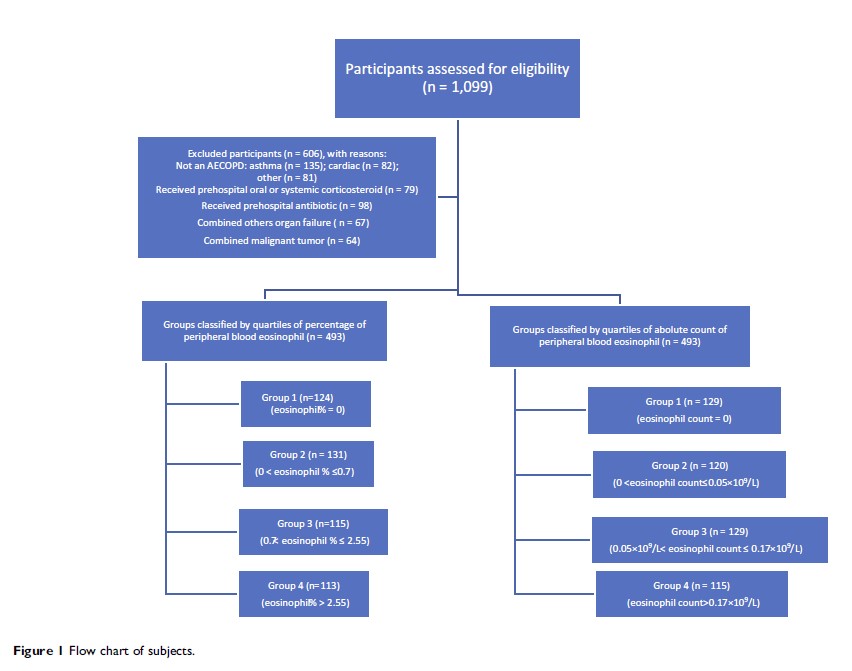
Methods: A prospective, multicenter, observational cohort study was performed in three teaching hospitals. Patients were grouped by quartile percentage (0, 0.7, 2.55) and absolute blood eosinophils count (0, 0.05×109/L, 0.17×109/L) and divided into four numbered groups ranked from low to high.
Results: The study included 493 AECOPD patients. In the percentile-ranked groups, patients in Group 1 experienced significantly longer hospital stays, higher rates of both noninvasive mechanical ventilation (NIMV), and heart failure than those in Group 4 (12 days vs 10 days, p = 0.005; 29.5% vs 23.6%, p = 0.007; 48.4% vs 28.5%, p = 0.001). Group 1 also had higher frequencies of respiratory failure and pulmonary heart disease compared to Groups 3 and 4 (54.8% vs 34.8%, p = 0.002; 54.8% vs 35%, p = 0.003). In the absolute count-ranked groups, patients in Group 1 had significantly higher rates of NIMV than those in Group 3 (41.1% vs 21.7%, p = 0.001), had higher rates of heart failure, respiratory failure, and pulmonary heart disease than those in Group 3 and 4 (48.1% vs 30.2%, p = 0.003; 48.1% vs 30.4%, p = 0.005; 50.8% vs 32.2%, p = 0.004; 50.8% vs 34.1%, p = 0.008; 51.9% vs 34.1%, p = 0.004; 51.9% vs 33%, p = 0.003). There were outcome differences among the admitting hospital of stays in the absolute count groups (p = 0.002), but the differences were not significant in a pairwise comparison. The proportion of ICU admissions and mortality was different in two cohorts with no difference in a pairwise comparison.
Conclusion: Patients with lower eosinophil counts experienced poorer clinical outcomes. Eosinophil levels may be a helpful marker to predict outcomes in AECOPD.
Keywords: eosinophils, chronic obstructive pulmonary disease, exacerbation, biomarkers, mortality