110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

较高的全身免疫炎症指数预示接受曲妥珠单抗辅助治疗的人表皮生长因子受体 2 阳性乳腺癌患者的低生存率
Authors Jiang L, Fang J, Ding J
Received 17 September 2019
Accepted for publication 24 December 2019
Published 21 January 2020 Volume 2020:12 Pages 475—484
DOI https://doi.org/10.2147/CMAR.S231444
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Dr Ahmet Emre Eskazan
Purpose: Neutrophils and platelets have been described as tumor-promoting factors, but lymphocytes have been described as tumor-inhibiting factors. The prognostic values of the neutrophil-to-lymphocyte ratio (NLR), and platelet-to-lymphocyte ratio (PLR) have been explored in human epidermal growth factor receptor (HER2)-positive breast cancer, however, the value of the systemic immune- inflammation index (SII) has not been studied in this molecular subtype. Our study aimed to compare the prognostic values of these inflammation-based indexes in Chinese HER2-positive breast cancer patients who received adjuvant trastuzumab.
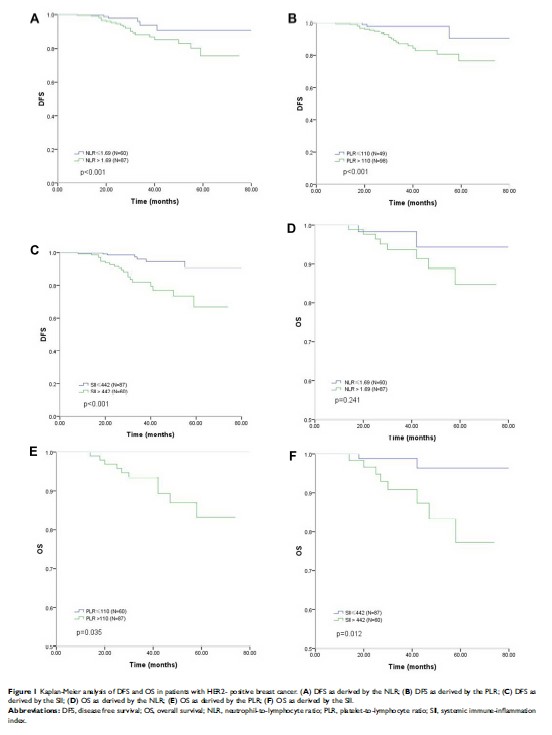
Methods: A total of 147 HER2-positive breast cancer patients were retrospectively analyzed. The association between clinicopathological factors and inflammation-based indexes was investigated. The Kaplan-Meier method was used to evaluate overall survival (OS) and disease-free survival (DFS); the Log rank test was performed to comparatively evaluate the survivals between the high-value and low-value groups. Multivariate Cox regression analysis was used to identify independent prognostic factors.
Results: The SII value correlated significantly with histological grade (HG)(p=0.016). The cut-off values determined by ROC analysis for the NLR, PLR and SII were 1.69, 110 and 442, and the corresponding areas under the curves (AUCs) were 0.621, 0.639 and 0.674, respectively. The 5-year DFS was significantly lower in the NLR-high than in the NLR-low group (75.8% vs. 90.7%, p< 0.01), in the PLR-high than in the PLR-low group (76.7% vs. 90.6%, p< 0.01) and in the SII-high than in the SII-low group (66.8% vs. 90.7%, p< 0.01). The 5-year OS was significantly lower in the PLR-high than in the PLR-low group (83.2% vs. 100%, p=0.035) and in the SII-high than in the SII-low group (77.3% vs. 96.4%, p=0.012). A multivariate regression model revealed that tumor size, lymph node involvement, HG, hormone receptor status, PLR and SII were independently correlated with DFS; lymph node involvement and SII were independently correlated with OS.
Conclusion: Our study suggests that SII is an independent prognostic factor for DFS and OS in HER2-positive breast cancer, and in terms of prognostic reliability, the SII is superior to other inflammation-based indexes.
Keywords: breast cancer, HER2, NLR, PLR, SII, prognosis