110932
论文已发表
注册即可获取德孚的最新动态
IF 收录期刊
- 3.4 Breast Cancer (Dove Med Press)
- 3.2 Clin Epidemiol
- 2.6 Cancer Manag Res
- 2.9 Infect Drug Resist
- 3.7 Clin Interv Aging
- 5.1 Drug Des Dev Ther
- 3.1 Int J Chronic Obstr
- 6.6 Int J Nanomed
- 2.6 Int J Women's Health
- 2.9 Neuropsych Dis Treat
- 2.8 OncoTargets Ther
- 2.0 Patient Prefer Adher
- 2.2 Ther Clin Risk Manag
- 2.5 J Pain Res
- 3.0 Diabet Metab Synd Ob
- 3.2 Psychol Res Behav Ma
- 3.4 Nat Sci Sleep
- 1.8 Pharmgenomics Pers Med
- 2.0 Risk Manag Healthc Policy
- 4.1 J Inflamm Res
- 2.0 Int J Gen Med
- 3.4 J Hepatocell Carcinoma
- 3.0 J Asthma Allergy
- 2.2 Clin Cosmet Investig Dermatol
- 2.4 J Multidiscip Healthc

非糖尿病人群的内脏脂肪指数和慢性肾病:一个横断面研究
Authors Xiao H, Xiong C, Shao X, Gao P, Chen H, Ning J, Chen Y, Zou Z, Hong G, Li X, You X, Sheng J, Wu F, Wang X, Zou H
Received 28 September 2019
Accepted for publication 15 January 2020
Published 4 February 2020 Volume 2020:13 Pages 257—265
DOI https://doi.org/10.2147/DMSO.S231656
Checked for plagiarism Yes
Review by Single-blind
Peer reviewer comments 2
Editor who approved publication: Dr Antonio Brunetti
Purpose: To investigate the correlation between visceral obesity and pathogenesis of chronic kidney disease (CKD) among non-diabetic individuals, and to evaluate the potential of visceral adiposity index (VAI) as a predictor of CKD.
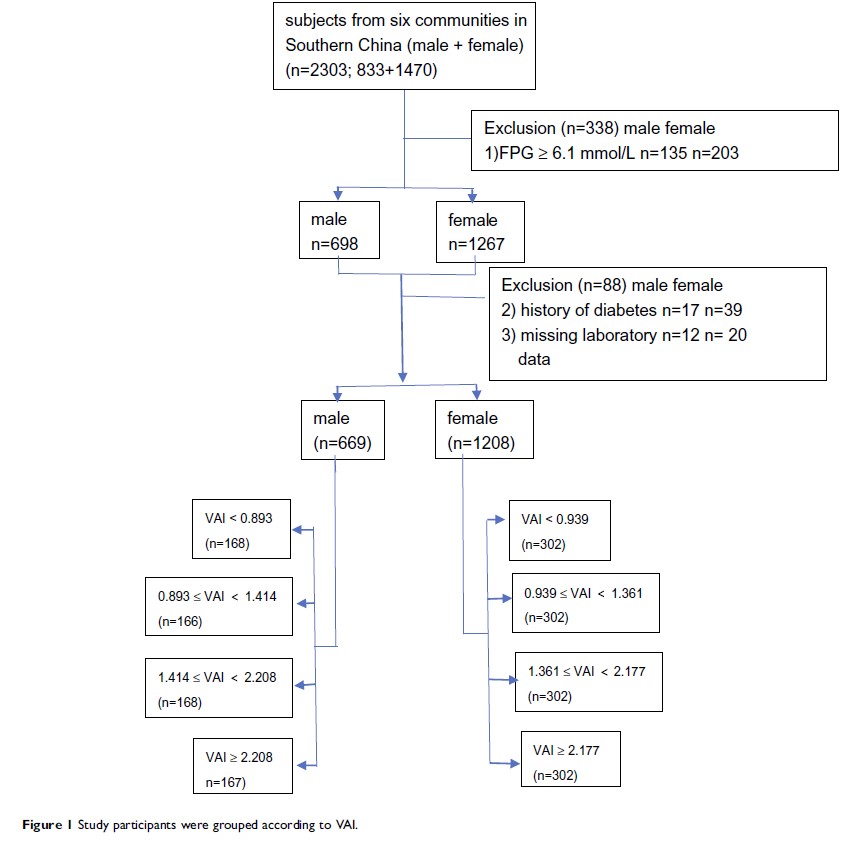
Patients and Methods: From December 2017 to March 2018, 1877 non-diabetic participants (male n=699, female n=1208) in southern China were recruited for a cross-sectional survey. Males and females were divided into four groups according to gender-specific quartiles of VAI scores. A logistic regression model was established to analyze the correlation between visceral adiposity index and CKD.
Results: Visceral adiposity index was positively correlated with CKD and was negatively associated with estimated glomerular filtration rate (eGFR). Using group one as the control, odds ratios (ORs) were calculated to determine the risk of developing CKD as VAI increased (male: group four 2.73 [P< 0.005]; female: Group three 1.76 [P< 0.05], Group four 2.88 [P< 0.005]). When related factors such as history of hypertension, smoking, alcohol use, and physical inactivity were normalized in the logistic model before calculation, ORs became 2.73 (male: P< 0.05), and 2.18 (female: P< 0.05), respectively. The results differed after normalizing further for systolic blood pressure (SBP), diastolic blood pressure (DBP), hypersensitive c-reactive protein (hsCRP), interleukin-6 (IL-6), homocysteine (Hcy), superoxide dismutase (SOD), and retinol-binding protein (RBP). There were no significant differences in ORs among the female groups.
Conclusion: Visceral adiposity index was significantly associated with CKD in non-diabetic individuals. It may be a good predictor of the pathogenesis of CKD and was dependent on hsCRP, IL-6, Hcy, SOD, RBP, and blood pressure levels in females and males with VAI scores of 1.41 and higher. Visceral adiposity index may be used to predict CKD in males with VAI less than 0.983.
Keywords: visceral adiposity index, chronic kidney disease, non-diabetic population